
Table of Contents
September Is Suicide Prevention & Awareness Month
Written By: Charlie Health Editorial Team
September 1, 2021
5 min.
September is National Suicide Prevention Month and here at Charlie Health, our goal is to dramatically reduce the skyrocketing rates of youth suicide and suicidal ideation in America. To highlight information and provide resources this month, keep reading to learn more about suicide, its warning signs, how to prevent it, and how to seek treatment.
Learn more about our Clinical Review Process
Table of Contents
WARNING: this post contains in-depth language and information about suicide and self-harm. If you are in acute crisis and looking for help, please call the National Suicide Prevention Lifeline at 988 or dial 911.
September is National Suicide Prevention Month, and here at Charlie Health, our goal is to dramatically reduce the skyrocketing rates of youth suicide and suicidal ideation in America. To highlight information and provide resources this month, keep reading to learn more about suicide, its warning signs, how to seek treatment, and how to support your family and loved ones who may be struggling.
Suicide facts
- From 2007 to 2018, the national suicide rate for young people aged 10-24 increased by 57%. This also reflects an increase in rates of suicide across the majority of states.
- In 2017, 6200 people aged 15-24 died by suicide, making it the second leading cause of death in this same demographic.
- In 2019, 18.8% of young people seriously considered suicide, while 8.9% attempted suicide.
- Females are more likely than males to attempt suicide.
- Black teenagers are more likely to attempt suicide than white teenagers.
- LGBTQ+ youth are disproportionately linked to suicide attempts.
Join the Charlie Health Library
Get mental health updates, research, insights, and resources directly to your inbox.
You can unsubscribe anytime.
Risk factors
- Pre-existing mental health disorders or psychiatric diagnoses, including major depressive disorder, bipolar, schizophrenia, borderline personality disorder, and PTSD
- Substance or alcohol abuse disorder
- Family history of suicide or attempted suicide
- History of trauma
- Easy access to lethal means of self-harm including firearms or prescription drugs
- Lack of access to mental health resources and health care
- Chronic illness
- Financial stress or loss
- Personal tragedies, including the loss of a parent, loved one, or a divorce
- Physical or sexual abuse
- Bullying
- Social isolation (this is an outsized concern given the ongoing coronavirus pandemic)
Reduction and prevention
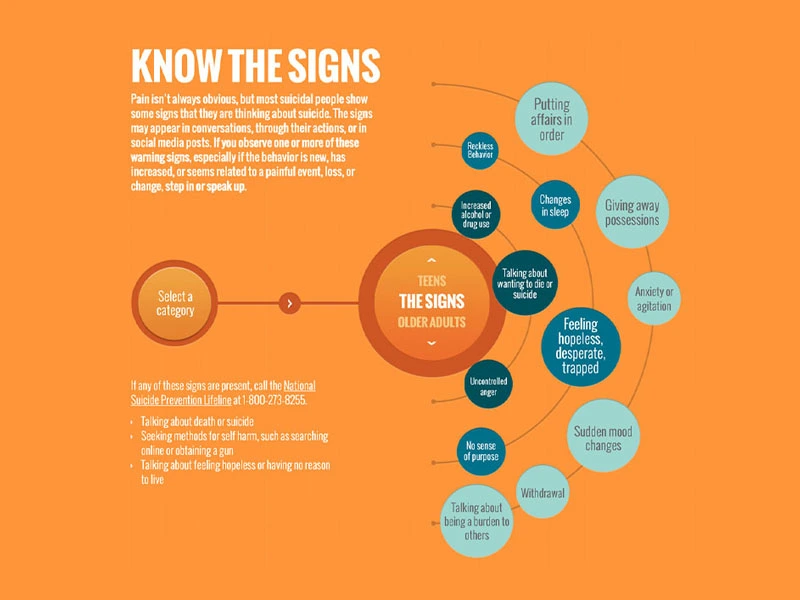
- Know the signs
- Reduce access to lethal tools of self-harm, including guns in the home or excess amounts of medication (especially opiates or other prescription drugs)
- Advocate and build resources for more access to mental health funding. This is one of the clearest ways to prevent suicide––when people know they have resources to rely on, they are more likely to reach out for help and be less afraid of the stigma.
Be proactive, not reactive
The more aware and attuned to changes in behavior we are, the more likely it is that we’ll be able to help prevent suicide. As many organizations dedicated to suicide prevention put it, “suicide is not inevitable.”
- Whether you’re a young person or a parent, fostering meaningful social connections is one of the best ways to combat suicide head-on.
- If you’re a young person, stay connected with your friends and family. As the school year is starting, try to sign up for a new extracurricular activity or make plans to see friends or study together (with pandemic safety measures, of course).
- If you’re a parent, keep talking to your kids even if they’re moody, disengaged, or resistant. You’re their advocate and number one source of love and support. They need you to pay attention and be patient as they navigate some of the toughest years of their lives in a very overwhelming, ever-shifting world.
- Identify when you or a loved one needs more help.
- Using the infographic above (and having a general sense of your own or your loved one’s general moods and tendencies), you should be able to discern when something is off. If that nagging feeling persists or intensifies, reach out for help. Charlie Health is one of many resources dedicated to helping people navigate thoughts of suicide and the continuity of care required once treatment is pursued. We are here to support, to answer questions, to offer a space of total non-judgment and unconditional love.
- If you or a loved one is experiencing thoughts of suicide, call the National Suicide Prevention Lifeline at 988 or dial 911. It’s never too soon to reach out.
Do you need more support with
your mental health?
Charlie Health can help.
Have a compassionate conversation
Here’s a script you can follow if you’re struggling with how to talk to a loved one about suicide.
- “I’ve noticed that you’ve mentioned feeling hopeless [like a burden, extremely depressed, tired] a lot lately. Sometimes when people feel like that, they’re thinking about suicide. Have you experienced thoughts of suicide/ending your life?”
- "I can imagine how tough this must be for you. I understand when you say that you aren't sure if you want to live or die. But have you always wanted to die? Well, maybe there's a chance you won't feel this way forever. I can help"
- "I'm deeply concerned about you, and I want you to know that help is available to get you through this."
- "Is there someone you can call if you think you may act on your thoughts of suicide?"
- "Do you have any weapons or prescription medications in the house?"
- "Please promise me that you will not harm yourself or act on any thoughts of suicide until you meet with a professional."
- [if applicable]: "Will you promise me that you will not drink or at least have someone monitor your drinking until we can get you help?"
What not to say
It’s just as important to avoid these questions and phrases as you approach someone you suspect is feeling suicidal. Alienating someone with dismissive or hostile language can be harmful and triggering; the same goes for enabling the secrecy and isolation of suicide ideation.
- "You're not thinking about suicide, are you?"
- “You're not thinking about doing something stupid, are you?"
- "Fine! If you want to be selfish and kill yourself, then go right ahead! See if I care."
- "Don't worry, I won't tell anyone. Your secret is safe with me."
Our mission at Charlie Health is to provide access to mental health services for as many high acuity patients as possible. Oftentimes, those who experience suicidal thoughts or have attempted suicide fall into this category. During this month, we encourage our families, patients, and anyone interested in reaching out to us to learn more about suicide, its warning signs, and its treatment options. By providing access to virtual intensive outpatient therapy options, we aim to reduce the gap in the continuum of care from emergency rooms to inpatient facilities and eventually back to home, school, or work. We believe that easy-to-reach, payer agnostic care paired with increased awareness and conversation around suicide is the best way to fight this endemic mental health crisis.
Contact us
Charlie Health’s team of licensed clinicians is here to support teens, young adults, and families struggling with mental health to process and navigate challenges together. Reaching out for help is a critical step in your journey toward healing. Professionals are available to listen to your needs, answer your questions, and match you with a treatment program that fits your needs. Get started today.
References
CDC: https://www.cdc.gov/nchs/data/nvsr/nvsr69/nvsr-69-11-508.pdf
United Health Foundation: https://www.americashealthrankings.org/explore/measures/teen_suicide
National Suicide Prevention Lifeline: https://988lifeline.org/how-we-can-all-prevent-suicide/
Suicide Awareness Voices of Education: https://save.org/about-suicide/mental-illness-and-suicide/
Suicide is Preventable: https://www.suicideispreventable.org/





