
Table of Contents
Treating Neurodivergence the Right Way: Personalized Care at Charlie Health

Written By: Elizabeth Kroll

Clinically Reviewed By: Dr. Kate Gliske
April 22, 2023
7 min.
Learn more about the neurodiversity movement and how Charlie Health is creating personalized treatment options for neurodivergent clients with comorbid conditions.
Learn more about our Clinical Review Process
Table of Contents
Neurodivergent youth and young adults experience high rates of comorbid psychiatric disorders, social isolation, and bias in school or the workplace. The last thing that we want is for our neurodivergent clients to feel out of place in the mental health field, which is why it’s important to not only understand what neurodivergence is, but also build affirming care for and with them.
Neurodivergence defined
In 1998, sociologist Judy Singer coined the term “neurodiversity” to describe the idea that everyone’s brain develops differently. This led to the neurodiversity movement, which promotes awareness and acceptance of neurodiverse conditions without viewing them as deficits.
Conditions that fall under the neurodivergent umbrella include, but are not limited to:
- ADHD
- Autism spectrum disorder (ASD)
- Dyslexia
- Dyscalculia
- Dyspraxia
- Learning differences
Because early research into neurodiversity was primarily done by non-neurodivergent individuals, these conditions were often described as “disabilities” that needed to be cured or fixed. This bias is often referred to as “ableism,” which is defined as a social prejudice against people with disabilities.
Today we can still see this ableist language used in the naming of these conditions: attention deficit hyperactivity “disorder” or autism spectrum “disorder”. The neurodiversity movement aims to move away from this ableist language and destigmatize neurodivergent differences as we learn more about them.
It is estimated that approximately 15-20% of the world’s population falls into at least one of the neurodivergent categories, with the most commonly discussed conditions currently being ADHD and ASD. In the United States, prevalence rates for both ADHD and ASD have been on the rise for the past two decades. However, diagnosis rates across different demographic groups remain uneven.
While the rate of ADHD diagnosis for boys between the ages of 5-17 is 14.6%, the rate of diagnosis for girls is only 6.9%, and similar discrepancies are found in ASD (4% of boys and 1% of girls).
Alternatively, neurodivergent identities tend to be more common in LGBTQIA+ communities, with one study finding that transgender and gender-diverse individuals were 3-6 times more likely to have an autism diagnosis than their cisgender counterparts.
Autism diagnosis or not, transgender and gender-diverse individuals are also more likely to score higher on self-reported measures of autistic traits such as sensory sensitivity. One hypothesis for this finding is that because individuals in the neurodivergent community are more familiar with questioning societal roles and identities, they apply the same curiosity and analysis to their gender and sexual identities.
Self-diagnosis and barriers to diagnoses
As society gains a better understanding and acceptance of neurodivergent conditions, self-diagnosis is becoming an increasingly relevant and intriguing topic.
Videos touting “5 signs you might be autistic” or “Neurodivergent memes without context” are a common trend on social media. While self-diagnoses in other mental health spheres is not recommended, the neurodiversity movement tends to support the self-diagnosis process, with some researchers even claiming it’s an important step to self-understanding and well-being for neurodivergent individuals.
Self-diagnosis within the community is often a product of barriers that people experience with receiving diagnoses, including:
- Anxiety
- Cost
- Access to adult specialists
- Fear of not being believed
- Inability to describe symptoms
- Mistrust of healthcare professionals
- Stigma
- The complexity of the healthcare system
- Lack of perceived value of formal diagnosis
Because there is no direct treatment or “cure” for neurodivergent conditions, people that self-diagnose often do not see the value in an “official” diagnosis.
One study participant that Laura Lewis interviewed claimed that “the expert didn’t tell me anything I didn’t already know.” Because self-diagnosis is supported, an official diagnosis is often not necessary for finding basic resources.
However, going undiagnosed with a neurodivergent condition has been associated with several risks, such as loneliness, isolation, underachievement at school, general unhappiness, and anxiety. It is still unclear in the literature whether self-diagnosis is a protective factor against these risks, but at the very least, self-diagnosis may help with self-understanding and community building.
Comorbidities and risks in neurodivergence
Autism, ADHD, and the multitude of other conditions that fall under the neurodivergent umbrella are correlated with a high rate of comorbid psychiatric disorders. Depression is among the highest comorbidities, with studies showing a comorbid rate with autism between 20% and 70% and a comorbid rate with ADHD of up to 50%. By comparison, approximately 12% of children in the general population are affected by major depression. Additionally, children with ADHD are at a much higher risk for adverse outcomes by mid-adolescence, including lower test scores, impaired school, family, and interpersonal functioning, and substance use disorders
ADHD and autism also tend to be highly associated with one another, with a comorbidity rate of 59%. It is currently contested to what degree ADHD and autism symptoms overlap, but some studies show that with in-depth psychological testing, ADHD and autism can be easily distinguished. In general, when autism and ADHD do co-occur, the symptom severity of each tends to be higher for all symptoms.
These comorbidities only emphasize the importance of de-stigmatizing neurodivergence, especially within the healthcare setting to allow individuals to receive affirming care that works for them and compliments the way they think and process. Affirming training and services are slowly becoming more prevalent within mental healthcare.
Treatment designed for neurodivergence at CH
(Co-written with Charlie Health Clinical Director Megan Lederman)
The neurodivergent clinical cohort at Charlie Health is designed to provide an opportunity for neurodivergent clients to connect in the context of an affirming clinical care experience.
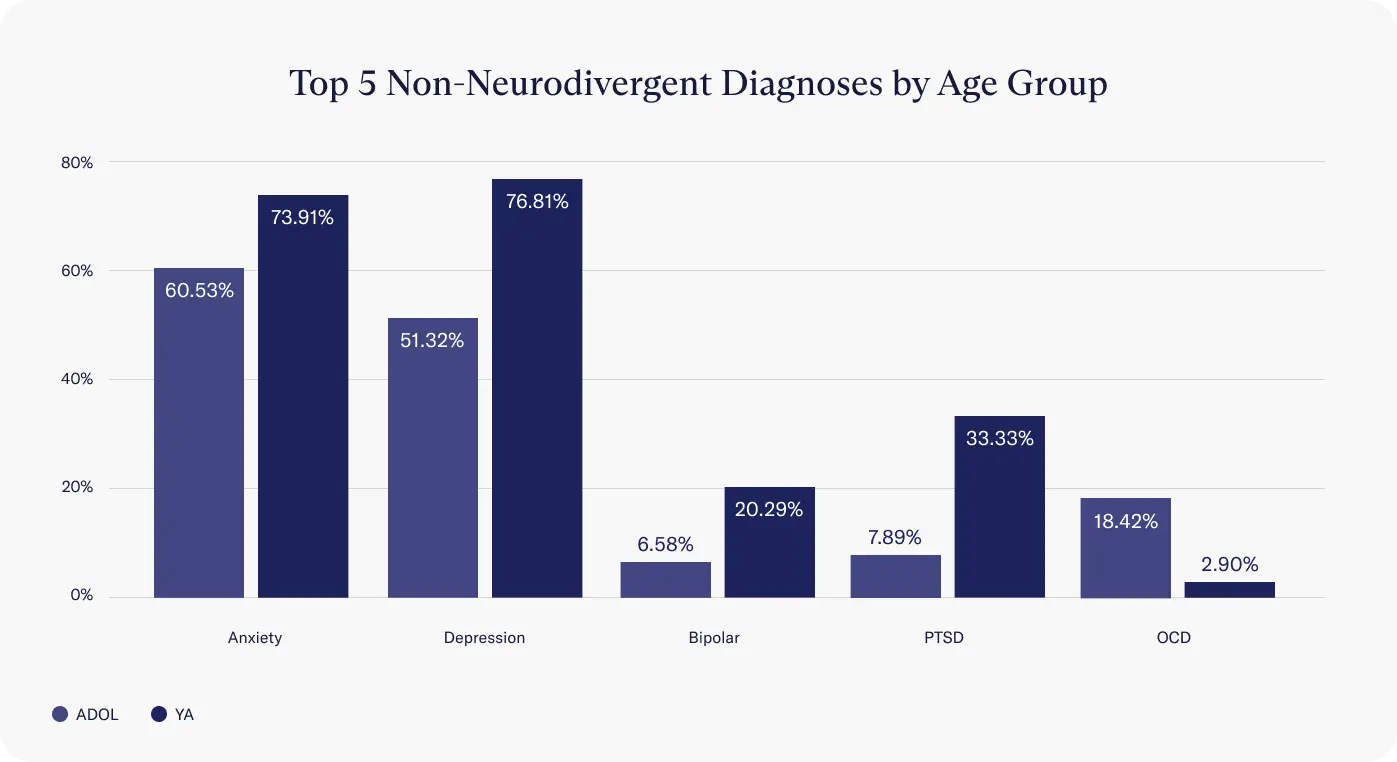
Our program is meant to address gaps in care accessibility for neurodivergent teens and young adults and to offer clients struggling with anxiety, depression, PTSD, and other mental health concerns a welcoming, empowering environment. This includes self-diagnosed neurodivergent clients.
A key factor in creating affirming care for our neurodivergent clients is placing them with peers who are experiencing similar challenges. Studies have shown that neurodivergent individuals have no communication deficits when talking to one another.
It is only when neurodivergent individuals and neurotypical individuals try to communicate that issues arise. By placing neurodivergent clients in groups together, we reduce the risk of clients feeling isolated or misunderstood.
The neurodivergent cohort is run by qualified facilitators with a curriculum that pairs an adapted, neurodivergent-friendly relational process hour with positive reinforcement-based behavioral therapies such as DBT skills and CBT.
This ensures that we provide a program of care that supports mental health symptom alleviation, decreased loneliness, and an increased sense of personal flourishing. Additionally, clients enrolled in our neurodivergent programming at Charlie Health have access to creative arts, contemplative, and experiential programming to enhance their care experience.
Our neurodivergent population
In a sample of 8273 young adults and adolescents admitted to Charlie Health, 151 have been a part of neurodivergent programming so far across our adolescent and young adult programs.
Diagnosed vs undiagnosed
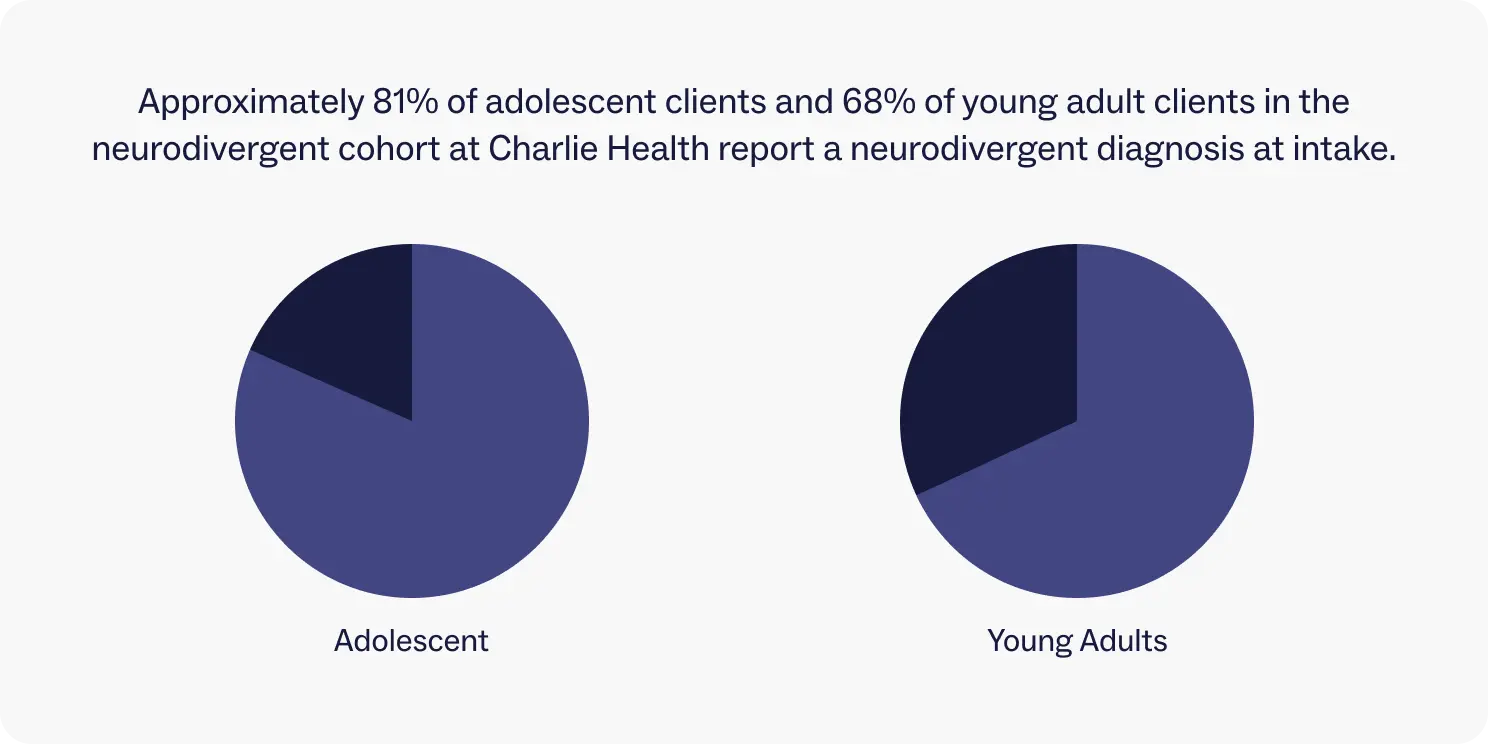
Because we allow self-diagnoses in the neurodivergent cohort, not all clients admit with an official diagnosis. Approximately 81% of adolescent clients and 68% of young adult clients in the neurodivergent cohort report a neurodivergent diagnosis at intake.
Diagnoses
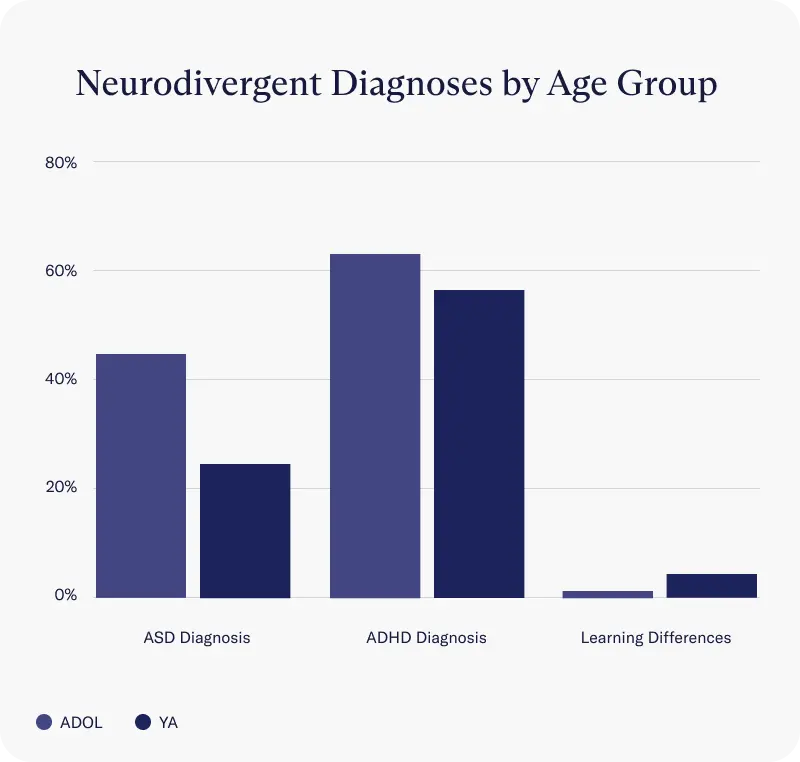
Within this cohort, ADHD and autism spectrum disorder are the most common neurodivergent diagnoses reported at intake. ADHD is also the 3rd leading concern for all clients that reach out to Charlie Health, after depression and anxiety.
Depression
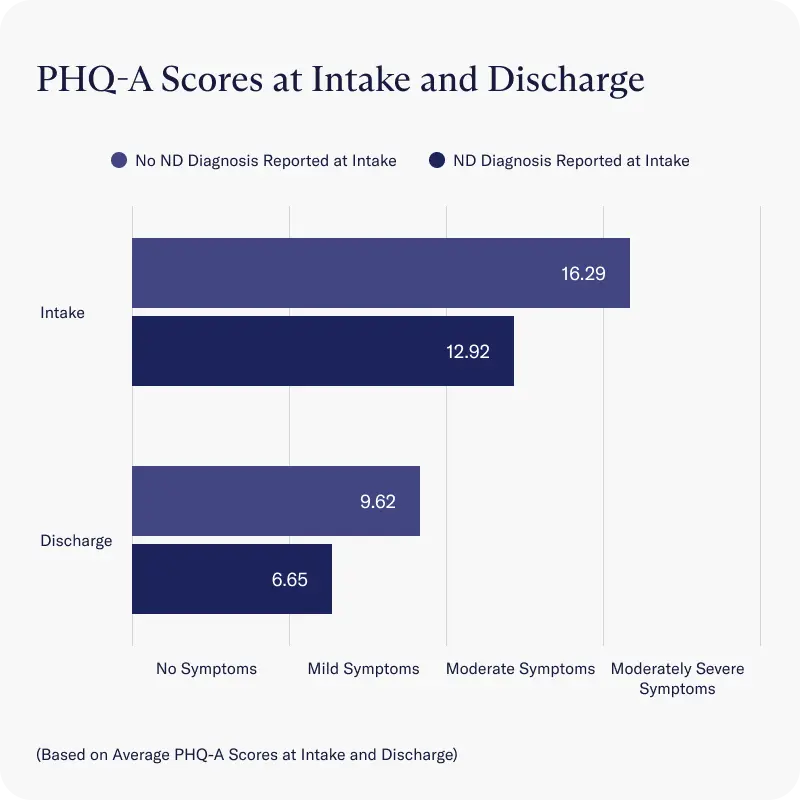
- Both neurodivergent groups and non-neurodivergent cohorts reported similar rates in depression severity at intake and discharge, as measured by average scores on the PHQ-A scale
- Across all clients, average depression severity decreased from moderate depression reported at intake to a score considered to be below the cut-point for major depressive disorder (PHQ-A sum score <10) by discharge.
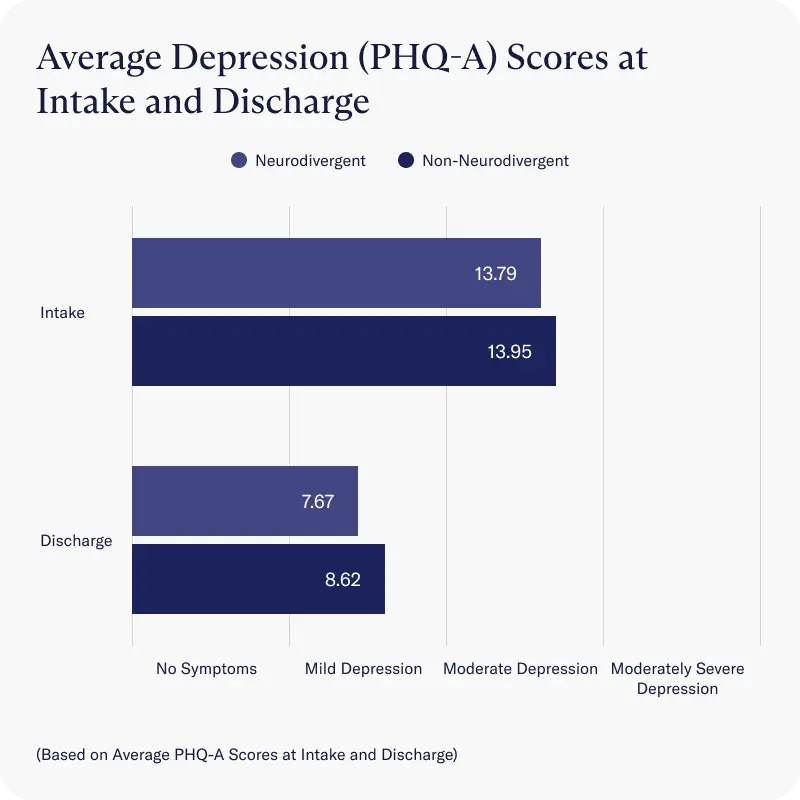
Clients in our neurodivergent cohort without an official neurodivergent diagnosis reported at intake reported significantly more severe depression than clients who had an official diagnosis at intake. However, at discharge, both groups had an average score considered to be below the cutoff point for major depressive disorder (PHQ-9 sum score <10).
Anxiety
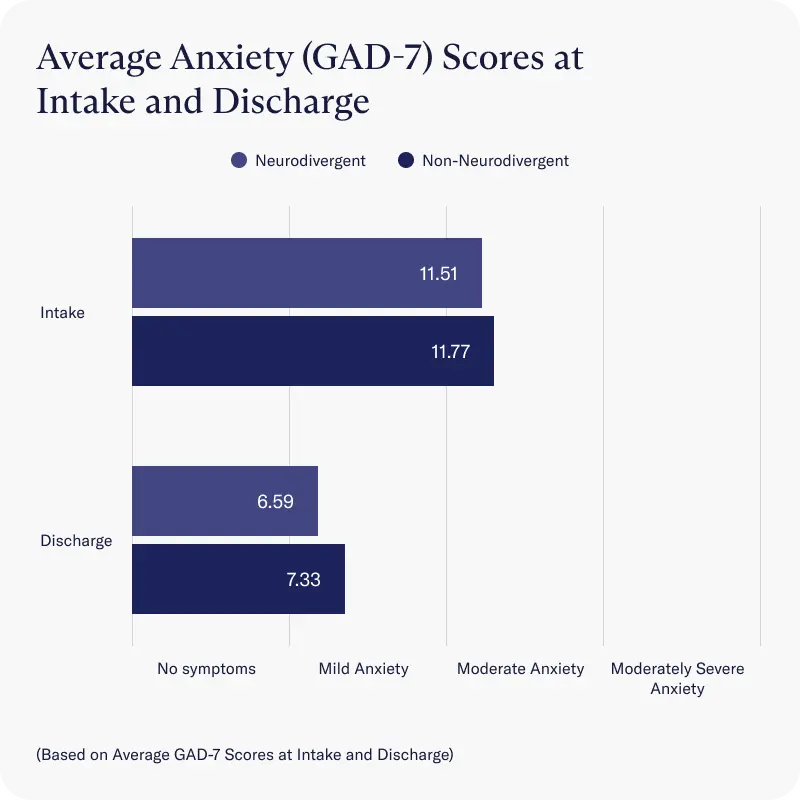
Both neurodivergent and non-neurodivergent cohorts reported decreases in anxiety symptoms that were statistically similar, as measured by average improvements on the GAD-7 scale. Both groups experienced a reduction from moderate to mild anxiety (GAD-7 sum score <9) by the time they were discharged.
Well-being
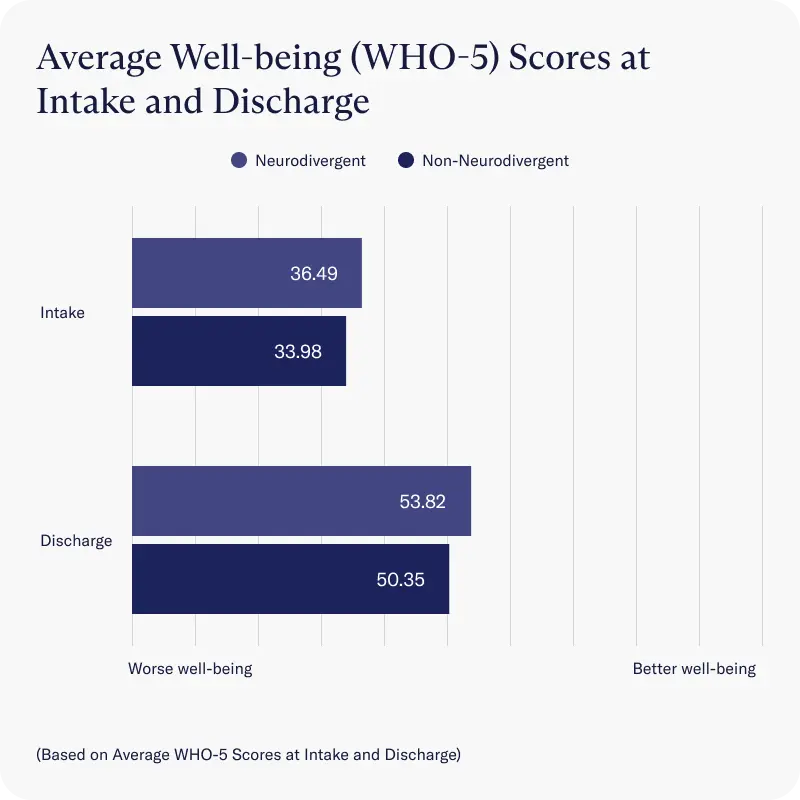
Similarly, neurodivergent and non-neurodivergent clients scored approximately the same on well-being at intake and made equitable improvements throughout the program, with both groups scoring outside of the well-being range considered for a depression diagnosis by discharge.
Conclusion
As neurodivergent conditions become more normalized in society, it is vital to provide safe and nurturing environments within the mental health sphere to promote well-being within the neurodivergent community.
The neurodivergent cohort at Charlie Health is an industry-leading program that adapts therapeutic methods for neurodivergent populations and produces positive outcomes for the members of our community, including anxiety and depression rates below the clinical threshold at discharge.


