
Table of Contents
New Research: Mental Health Engagement Data Can Help Personalize Care

Written By: Alex Bachert, MPH

Clinically Reviewed By: Dr. Don Gasparini
September 7, 2023
6 min.
A recent quality improvement analysis from Charlie Health studied the types of youth who participate in virtual intensive outpatient programming (IOP) and their risk factors for disengagement. Learn how this information can help personalize future care for teens and young adults.
Learn more about our Clinical Review Process
Table of Contents
The mental health crisis continues to affect youth across the country, with nearly 20% of teens and young adults living with mental health conditions. Research suggests that access to psychiatric treatment can effectively reduce symptoms and improve quality of life, so why are so many teens and young adults still struggling to manage their mental health? One possible reason are high dropout rates from treatment, particularly among young people.
In order to understand how to increase treatment engagement and improve outcomes among teens and young adults, a team of researchers conducted a quality improvement analysis of the types of youth who seek intensive outpatient programming (IOP) support and their risk factors for disengagement. You can read the full publication here.
“Treatment providers have been working for decades to unlock the key to personalizing treatment engagement strategies within large systems of care. Attention to treatment engagement and who drops out of treatment is also critical for effective research and evaluation, as clients who drop out often have distinct features and outcomes from those who remain,” wrote the researchers.
“The implications of this research provide a blueprint for how other treatment programs might use their own data to track treatment engagement and personalize care within their program,” commented Elizabeth Kroll, Charlie Health’s RCO Senior Outcomes Analyst.
Below, we dive deeper into the study methods, results, and suggestions for improving treatment engagement rates among teens and young adults.
A look at the research: methods and results
Charlie Health’s Research and Clinical Outcomes team analyzed self-reported variables and administrative data from nearly 3,000 teens and young adults discharged from Charlie Health’s virtual IOP between July 2021 and February 2023.
Engagement outcomes were measured in three ways: total number of groups attended, treatment completion, and disengagement from treatment before completing treatment goals. Treatment completion was defined as completing treatment goals and being routinely discharged. Disengagement, on the other hand, was defined as being discharged from treatment against clinical recommendation or without completing treatment goals.
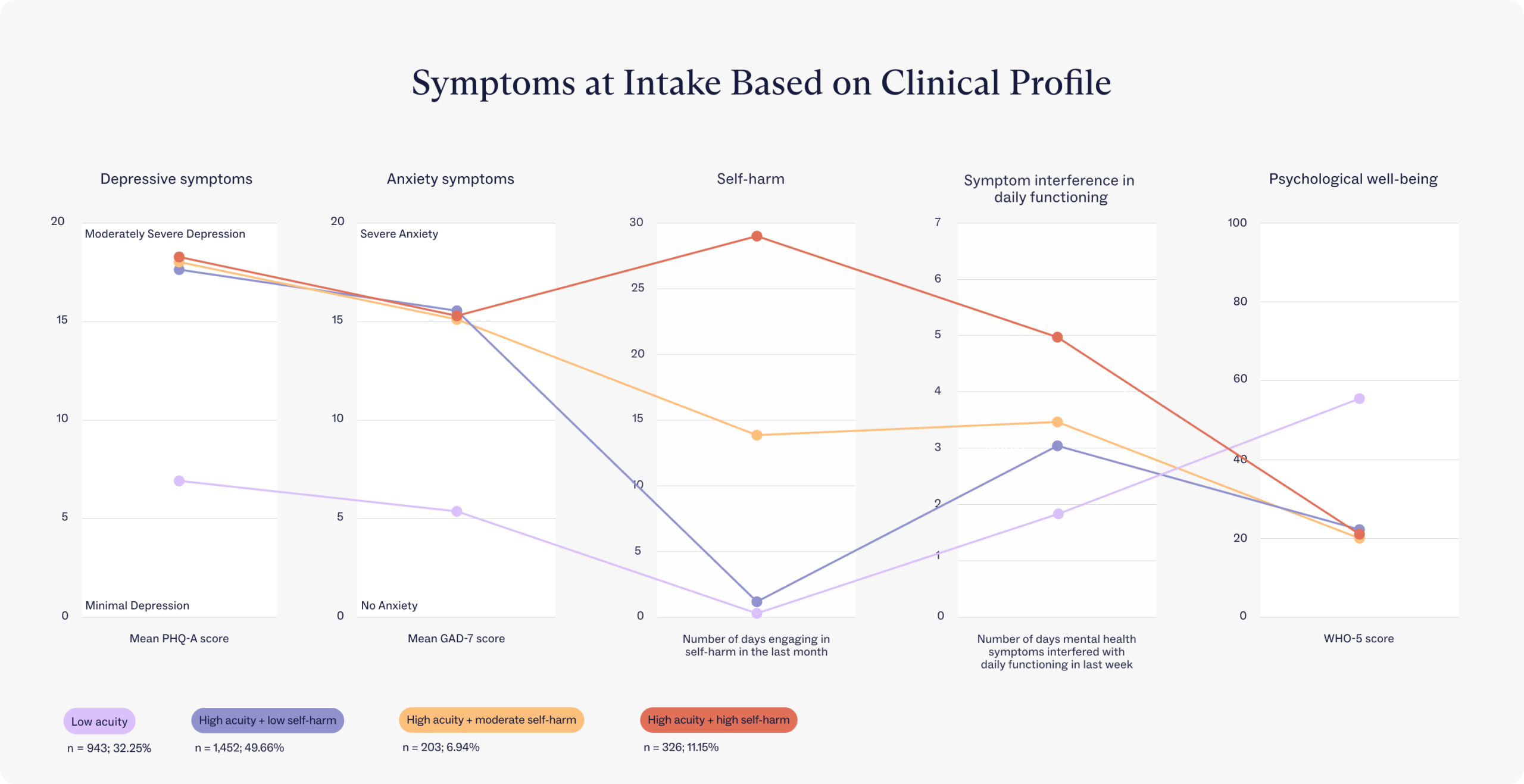
Using five variables that youth reported at intake (depression, anxiety, well-being, days of self-harm, and impact on daily functioning), the researchers identified four acuity profiles to determine patterns in treatment engagement outcomes.
Low acuity
High acuity + low self-harm
High acuity + moderate self-harm
High acuity + high self-harm
Young people who didn’t have much of a tendency to self-harm and whose mental health symptoms (including mild depression and anxiety) interfered with daily functioning less than 2 days per week.
Young people who didn’t have much of a tendency to self-harm but whose severe mental health symptoms (including moderate depression and severe anxiety) interfered with daily functioning about 3 days per week.
Tab content: Young people who self-harmed about half of the days in the last month and whose severe mental health symptoms (including moderate depression and severe anxiety) interfered with daily functioning for about half the week.
Young people who self-harmed nearly every day in the last month and whose severe mental health symptoms (including severe depression and anxiety) interfered with functioning almost daily.
1. Low acuity
This group consisted of youth who reported mild levels of depression and anxiety and minimal self-harm. They noted that their mental health symptoms meaningfully interfered with their daily functioning, but usually less than 2 days per week.
2. High acuity + low self-harm
Teens and young adults who reported moderately severe depression and severe anxiety and lower levels of psychological well-being compared to the low acuity profile. They noted minimal self-harm and that their mental health symptoms interfered with their daily functioning approximately 3 days per week.
3. High acuity + moderate self-harm
Teens and young adults who reported moderately severe depression, severe anxiety, and low levels of psychological well-being. They self-harmed approximately half of the days in the last month, and their mental health symptoms interfered with their daily functioning about half of the week.
4. High acuity + high self-harm
This group consistently had the poorest clinical and functional outcomes across all the profiles, with the lowest levels of psychological well-being. These young people reported moderately severe depression and severe anxiety, engaged in self-harm nearly every day in the last month, and reported the highest levels of interference with their daily functioning.
It’s important to note that this is the first study of its kind to include self-harm, which was a distinguishing feature between the four groups. For example, the low acuity and high acuity + low self-harm groups both reported very little self-harm but had significantly different levels of depression and anxiety at intake. The researchers also found that those who reported daily self-harm had the highest rates of treatment completion and the lowest levels of early disengagement compared to the other groups.
The research yielded several other notable findings:
- Teens and young adults in the low acuity and high acuity + low self-harm profiles attended an average of 4-5 fewer treatment sessions compared to those in the high acuity + moderate self-harm and high acuity + high self-harm profiles.
- Individuals in the high acuity + low self-harm group completed treatment at a significantly lower rate compared to the other two high acuity profiles.
- Those in the high acuity + high self-harm profile were significantly less likely to disengage or end treatment early compared to all other profiles.
- Youth who identify as LGBTQIA+ were significantly more likely to be classified into one of the high acuity profiles compared with the low acuity profile, suggesting significantly higher acuity for these populations compared to their cisgender, heterosexual peers.
Three takeaways for future youth mental health treatment
“Identifying subgroups that differentially engage in treatment is a critical first step towards personalizing treatment within complex populations,” explained the researchers. According to their findings, several takeaways can be used to proactively assign clients to clinical programming that’s the right fit for their needs.
1. Create additional engagement strategies for high acuity + low self-harm youth
Youth with severe depression and anxiety but minimal reports of self-harm were less likely to complete treatment than the other two high acuity groups, suggesting that this group may benefit from additional resources or engagement strategies.
2. Focus on groups other than the high acuity + high self-harm group
The researchers found that youth in the high acuity + high self-harm profile completed treatment at a significantly higher rate compared to youth in all other groups. This suggests that Charlie Health currently employs effective engagement strategies for those with moderately severe depression, severe anxiety, and frequent self-harm, and greater attention should be focused on the other groups.
3. Design more programs for LGBTQIA+ youth
The analysis found that youth identifying as sexual or gender marginalized populations were more likely to be classified into high acuity groups (meaning moderately severe depression and severe anxiety ). This suggests that these groups — more specifically, non-binary, transgender, bisexual, and pansexual young people — may benefit from additional resources targeting specific issues, including ways to cope with stress, depression, and anxiety.

Life-saving outcomes. Industry-leading care.
Learn more about our research and clinical outcomes.
Why do engagement rates matter?
People choose to drop out of mental health treatment for different reasons. Some people leave early because they’ve noticed improvements and believe they’re ready, while others disengage due to changes in motivation, perceptions of usefulness, or a lack of stability in their lives.
Regardless of the reason, research shows that folks who leave mental health treatment early or attend fewer sessions may not receive the full benefits of their care. For example, people who drop out early are less likely to see significant improvements with their depression or anxiety, have smaller reductions in trauma symptoms, and are less likely to maintain improvement.
Without adequate treatment, mental health challenges can lead to other short-term and long-term consequences for teens and young adults — such as dropping out of school, unemployment, substance abuse, self-harm, and violence.
Start treatment today with Charlie Health
Charlie Health is on a mission to end the youth mental health crisis through equitable access, evidence-based care, and life-saving research. Through our virtual Intensive Outpatient Program (IOP), we offer client-centered care to help all teens and young adults proactively achieve their mental health goals.
Our clinicians are trained in leading evidence-based family therapy sessions and have the opportunity to consult frequently with family therapy experts so that your family is always in the best hands. No matter where you are in your mental health journey, we’re here to support you with a customized treatment plan based on your unique needs. Fill out this short form to get started today.
References

