
Table of Contents
New Research: Virtual Care Improves LGBTQIA+ Youth Mental Health

Written By: Alex Bachert, MPH

Clinically Reviewed By: Dr. Kate Gliske
June 1, 2023
5 min.
Access to LGBTQIA+ specific programming improves depression and reduces suicide risk, though additional resources may benefit transgender youth.
Learn more about our Clinical Review Process
Table of Contents
The United States is currently experiencing a nationwide youth mental health crisis. The effects are widespread, but the problem is particularly pronounced in the LGBTQIA+ community, with LGBTQIA+ youth facing disproportionately high levels of depression, self-harm, and suicidal thoughts and behaviors compared with their non-LGBTQIA+ peers.
For those who aren’t familiar with the term, LGBTQIA+ stands for lesbian, gay, bisexual, transgender, queer, questioning, intersex, and asexual/aromantic/agender, “plus” all other identities along the gender and sexuality spectrum.
Despite the alarming mental health trends among LGBTQIA+ youth, there’s still a shortage of psychiatric providers, treatment programs, and outcomes research focused on this population. To help address this disparity, Charlie Health conducted a study to assess the potential role of identity-affirming and culturally competent care in achieving equitable outcomes for our most vulnerable youth.
Led by Dr. Caroline Fenkel DSW, LCSW, Co-Founder and Chief Clinical Officer at Charlie Health, and Dr. Kate Gliske, Director of Research & Clinical Outcomes, the team studied data from Charlie Health’s virtual Intensive Outpatient Program (IOP) to understand:
- Were LGBTQIA+ youth and young adults more clinically severe at program intake and discharge compared to non-LGBTQIA+ patients?
- Did LGBTQIA+ youth and young adults participating in LGBTQIA+-specific programming experience clinically significant changes between intake and discharge?
- Were there any notable differences among subgroups, such as transgender or nonbinary youth?
Read the full publication here.

Industry-leading care for LGBTQIA+ youth.
Outcomes that speak for themselves. Treatment that saves lives.
The research participants
The study included 880 teens and young adults, with more than half (551) identifying as LGBTQIA+. All participants attended 5 or more Charlie Health IOP sessions and were discharged from the program between December 2020 and May 2022. Approximately half of LGBTQIA+ youth reported having one LGBTQIA+ identity, and one-third reported two intersectional LGBTQIA+ identities.
At the start of treatment, LGBTQIA+ youth were more likely than non-LGBTQIA+ to report:
- Active suicidal ideation
- Passive suicidal ideation
- History of suicide attempts
- Clinical non-suicidal self-injury
- Significantly worse depression
The findings: promising results for LGBTQIA+ mental health
The researchers concluded that psychiatric programming designed specifically for the LGBTQIA+ community is an effective solution for meeting the elevated mental health needs of LGBTQIA+ youth.
Here’s what they found.
Although many LGBTQIA+ youth exhibited severe mental health symptoms at the start of treatment, they showed considerable clinical improvements in depression, suicide risk, and self-harm between starting and ending the virtual IOP.
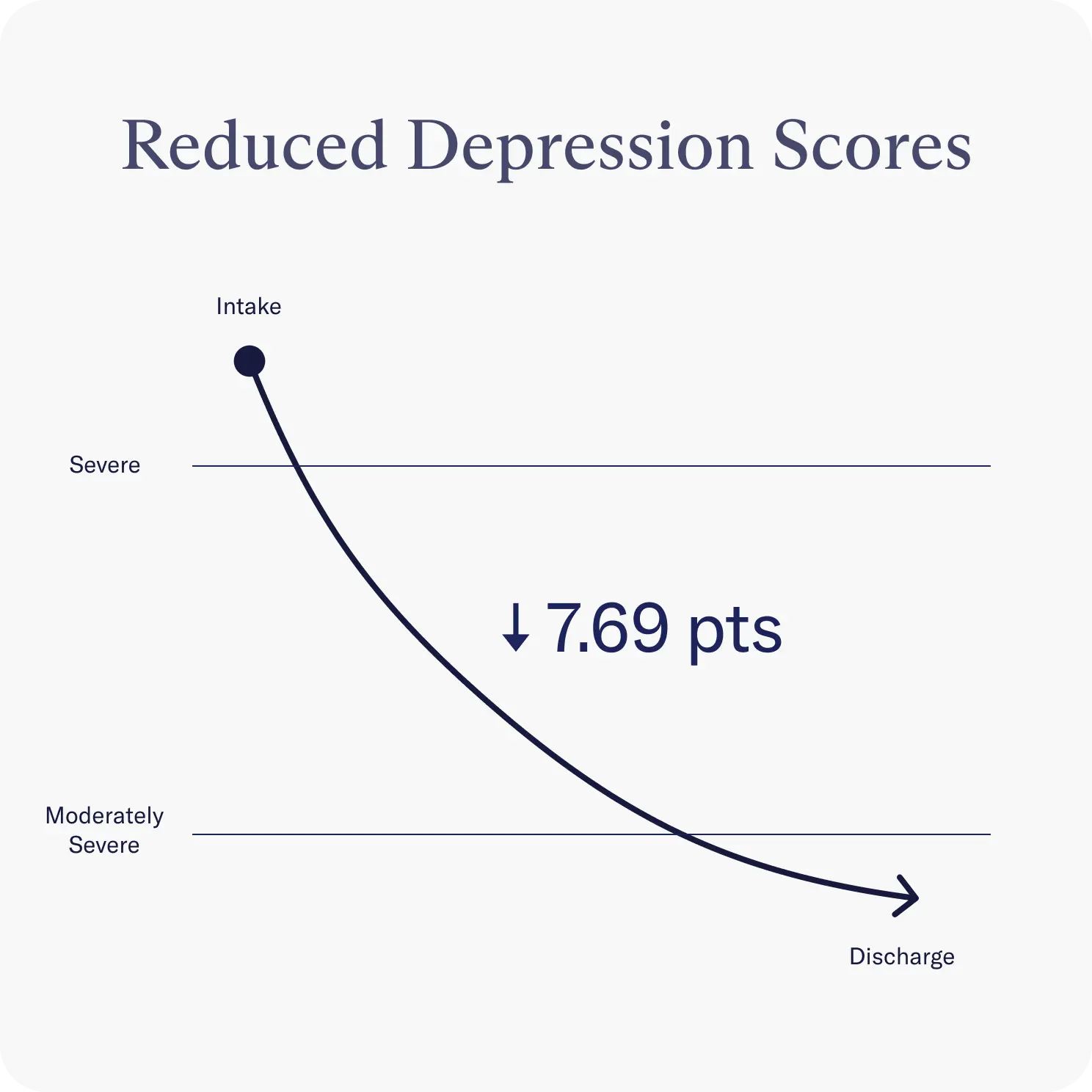
Reduced depression scores
The researchers used a multiple-choice, self-reported questionnaire called the PHQ-A to monitor depression severity. Among LGBTQIA+ youth who met the criteria for depression at the start of treatment (379 out of 551 individuals), PHQ-A scores improved by an average of 7.69 points. To translate, this represents a clinically significant change from a moderately severe level of depression to a moderate level of depression.
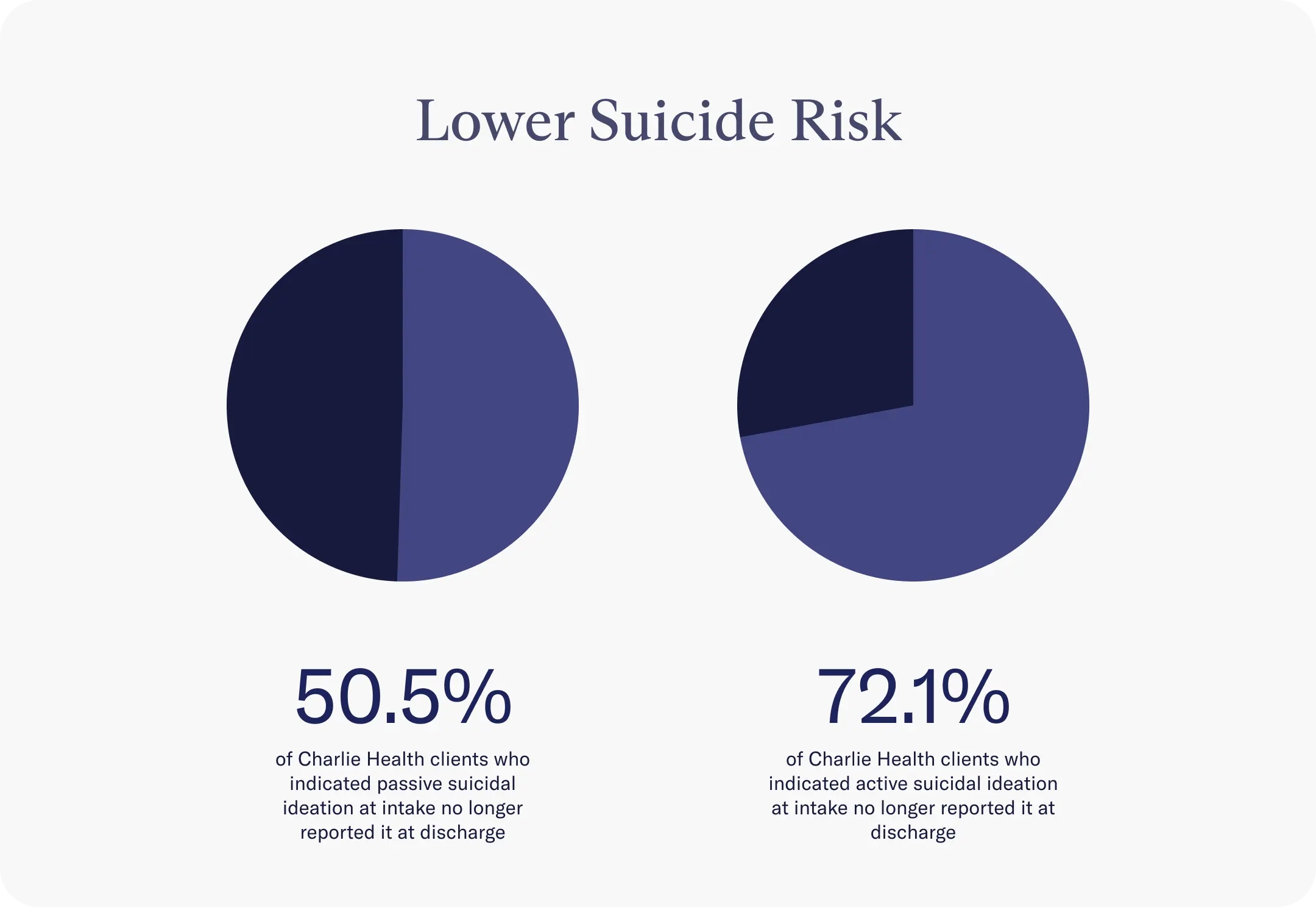
Lower suicide risk
The researchers studied both passive and active suicidal ideation. Passive suicidal ideation is when a person has thoughts of self-harm or suicide but doesn’t intend to act on those impulses, while active suicidal ideation suggests thoughts of self-harm or suicide and a plan to carry them out.
Overall, the youth reported a reduction in passive and active suicidal ideation. More specifically:
- 50.5% of LGBTQIA+ youth who indicated passive suicidal ideation at the start no longer reported it at discharge
- 72.1% of LGBTQIA+ youth who indicated active suicidal ideation at the start no longer reported it at discharge
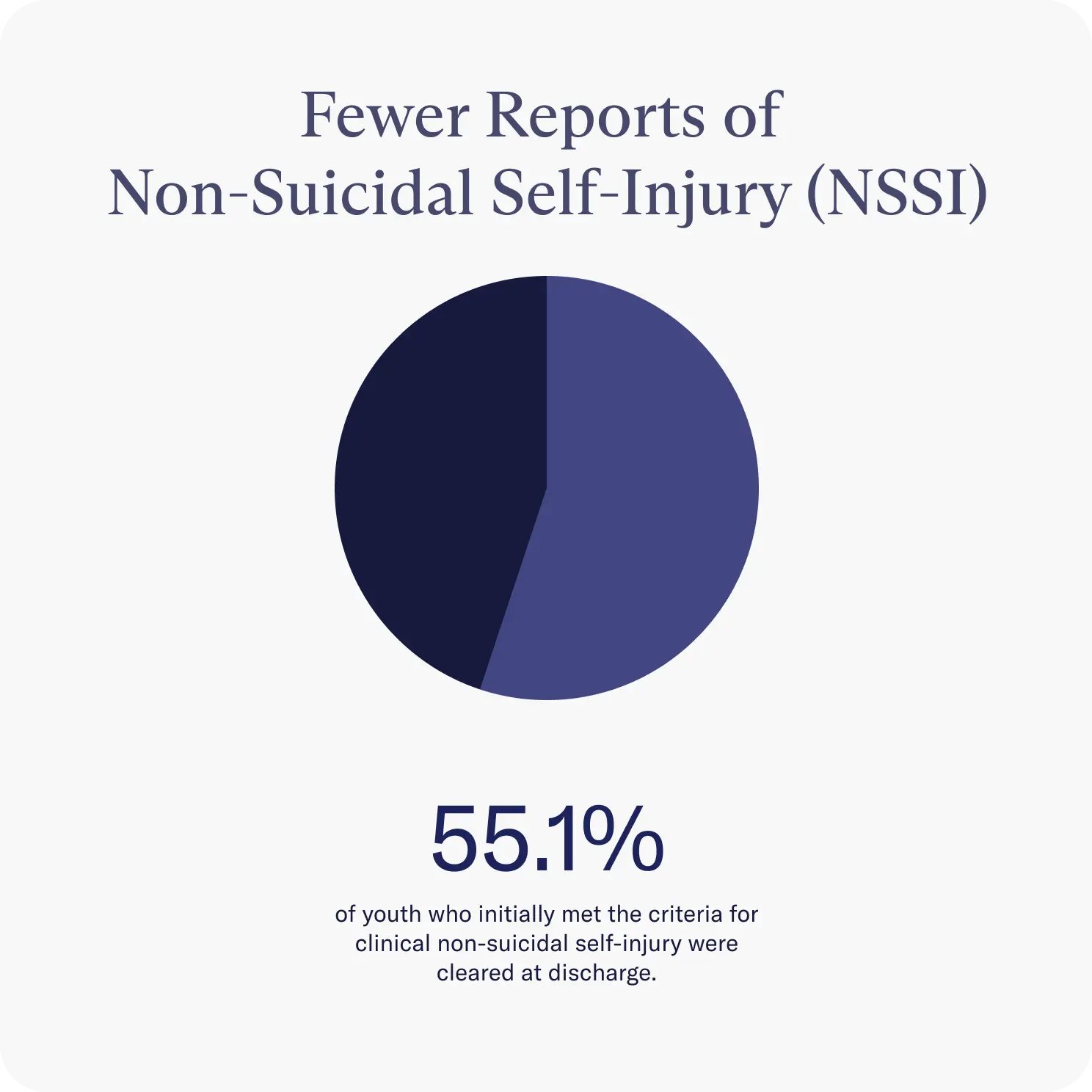
Fewer reports of non-suicidal self-injury (NSSI)
Similar improvements were noted in the area of non-suicidal self-injury. By the end of treatment, 55.1% of youth who initially met the criteria for clinical non-suicidal self-injury were cleared. In order to assess NSSI, the researchers used a tool called Alexian Brothers Assessment of Suicidal Ideation (ABASI) which includes 21 different types of self-injury. Respondents are asked to indicate how many days in the past 30 days they engaged in any behaviors, with behaviors on five or more days classified as clinical non-suicidal self-injury.
Transgender youth still face inequities
Although the programming showed improved mental health outcomes among LGBTQIA+ youth, there were still certain populations that might benefit from additional support. Transgender and nonbinary youth had greater non-suicidal self-injury within the LGBTQIA+ group, and a subgroup analysis found that transgender youth were:
- 1.8 times more likely to report active suicidal ideation at discharge
- 2 times more likely to report clinical non-suicidal self-injury at discharge
The takeaway
According to the National Alliance on Mental Illness, various risk factors may contribute to the disproportionate rate of poor mental and behavioral health outcomes among LGBTQIA+ teens and young adults. These include:
- Coming out/ inviting in
- Trauma
- Substance abuse
- Homelessness
To date, most research on mental health outcomes focuses exclusively on adults, with very limited data on treatment outcomes for LGBTQIA+ youth. One reason for this research shortage is an overall lack of programming for this specific population.
“In order to adequately address a public health issue as complicated and diverse as the youth mental health crisis, providers must do more than just increase the availability of care, but also ensure the development and wide-spread availability of identity-affirming and culturally competent care in order to ensure equitable outcomes for our most vulnerable youth,” wrote the researchers.
They concluded that more LGBTQIA+-specific programming is needed, specifically for transgender youth, and virtual programs can help meet the demand.
Join the Charlie Health Library
Get mental health updates, research, insights, and resources directly to your inbox.
You can unsubscribe anytime.
Find LGBTQIA+ mental healthcare with Charlie Health
Charlie Health offers the first virtual program designed to address acute and severe depression, self-harm, and suicidality in LGBTQIA+ adolescents and young adults. Our team of compassionate professionals is dedicated to providing a safe space to help people explore their sexuality, navigate their gender identity, and treat their mental health concerns.
Charlie Health offers comprehensive mental health treatment for adolescents, young adults, and their families. Our virtual Intensive Outpatient Program (IOP) combines individual therapy, group sessions, family therapy, and psychiatric support to create a personalized treatment plan based on your unique background, preferences, and mental health needs.
Contact us today to start your journey toward mental wellness.
References
https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-017-1337-8
https://www.nami.org/Your-Journey/Identity-and-Cultural-Dimensions/LGBTQI
https://journals.sagepub.com/doi/10.1177/0886260517718830
https://www.tandfonline.com/doi/full/10.1080/00981389.2016.1193099
https://www.charliehealth.com/post/inviting-in-coming-out-101
https://www.charliehealth.com/post/what-is-lgbtqia-counseling




