Table of Contents
How Trauma Affects the Brain

Written By: Ashley Laderer

Clinically Reviewed By: Dr. Don Gasparini
January 17, 2023
7 min.
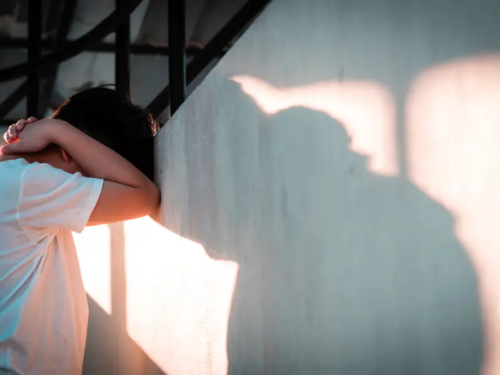
Trauma doesn’t just cause changes to your emotions––it also is scientifically proven to change your brain. Here’s how trauma affects the brain, and what that means for you.
Learn more about our Clinical Review Process
Table of Contents
How trauma affects the brain
Trauma doesn’t just affect your feelings––it literally changes your brain, too. Before diving into exactly how trauma affects the brain, it’s important to understand a few regions of your brain and why they are important in relation to psychology and mental health.
The amygdala
The amygdala is the part of your brain that’s most linked to emotions and fear. It is responsible for emotional learning, emotional memories, and fear conditioning, to name a few of its important jobs. When the amygdala senses a threat, it can send signals to another part of your brain called the hypothalamus, which could then trigger a fight, flight, freeze, or even fawn response.
The hippocampus
The hippocampus is important for your memory and learning. It helps you form new memories and store long-term memories. It’s also tied to emotions and stress.
The prefrontal cortex
The prefrontal cortex has many important roles when it comes to brain function, including decision-making, memory, learning, attention, problem-solving, and creativity.
These three brain regions are crucial for your overall functioning and well-being. However, research has shown that traumatic stress can result in long-term adverse changes to those very regions.
For example, trauma can cause the amygdala to become hyperactive, or more sensitive than the average amygdala. That means someone who’s experienced trauma may be more on edge, easily startled, or hypervigilant. Threats may feel even more dangerous than they are, and they may be sent into fight-or-flight more easily.
Trauma can result in a smaller hippocampus, particularly in the case of childhood trauma where the events occurred while someone’s brain was still developing. Nonetheless, since the hippocampus is important for memory, there may be some overlap with PTSD symptoms since PTSD often results in recurring distressing memories or flashbacks.
Furthermore, since the prefrontal cortex is linked to executive functioning, and since this region may be negatively impacted by trauma, some research shows that people with PTSD have impaired executive functioning.

How childhood trauma affects the brain
Trauma at any stage of life can affect the brain. However, if trauma occurs during childhood while the brain is still developing, the effects may be more pronounced. Brain development isn’t fully complete until someone is in their mid-to-late 20s. This is particularly true for the prefrontal cortex region which is one of the final regions of the brain to reach full maturity.
While trauma can affect the brain at any age, it can be particularly detrimental during the times when your brain is supposed to be developing “normally.”
For example, research has found the following effects of childhood trauma on the brain:
- It can disrupt the normal stress response.
- It can affect the function of neurotransmitters (which essentially act as chemical messengers in the brain) such as cortisol, dopamine, and norepinephrine.
- Higher levels of cortisol (the stress hormone) due to trauma can affect the way that brain regions such as the prefrontal cortex mature.
- It can cause the hippocampus (the part of the brain associated with learning) to be smaller.
- It can cause the amygdala to become hyperactive.
These brain changes due to childhood trauma can lead to various potential struggles for a child or teen, including:
- Trouble focusing or paying attention
- Learning disabilities
- Lower self-esteem
- Trouble with social skills
- Difficulty with sleep
- Mental health conditions such as anxiety, bipolar disorder, depression, PTSD, and substance use disorder
- Increased risk for suicidal behavior
Trauma-related mental health conditions
Not everyone who experiences trauma goes on to develop a mental health condition, but some do. The two main possible mental health outcomes are acute stress disorder (ASD) and post traumatic stress disorder (PTSD).
As the name suggests, acute stress disorder is an “acute” or short-term condition. If you have ASD, your symptoms will last for at least three days or up to a month after the trauma exposure. Around 6% to 33% of trauma survivors develop acute stress disorder. In order to be diagnosed with ASD, you must meet specific diagnostic criteria outlined by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).
Some examples of acute stress disorder symptoms are:
- Recurring distressing memories or dreams
- Intense flashbacks
- Low mood
- Dissociating
- Avoidance of triggers
- Being hypervigilant or on edge
- Difficulty with sleep
- Irritability
Do you need more support with
your mental health?
Charlie Health can help.
Post traumatic stress disorder is a longer-term mental health condition. PTSD doesn’t necessarily come on right after a traumatic experience. In some cases, you might not develop PTSD symptoms until even years later. Around one-third of people who experience intense trauma have PTSD.
Like ASD, there are specific diagnostic criteria in the DSM-5 for someone to be diagnosed with post traumatic stress disorder. PTSD symptoms are similar to ASD. Examples of symptoms include:
- Recurring distressing memories or nightmares
- Flashbacks where you may feel like the incident is happening now
- Having physical symptoms when you’re triggered by something related to the traumatic event
- Avoiding internal reminders (like memories and thoughts) and external reminders (like places or people) that make you think of the traumatic event
- Consistently feeling negative emotions
- Feeling detached from others
- Loss of interest in activities and inability to feel pleasure
- Anger, aggression, and irritability
- Being hypervigilant and easily startled
Furthermore, people with PTSD often have co-occurring mental health conditions including:
- Anxiety disorders
- Depression
- Substance use disorder
Treatment for trauma and related conditions
Mental health treatment can be extremely helpful to process your trauma, discover coping mechanisms, move forward, and grow after a traumatic instance or instances. The key to trying to prevent ASD and PTSD is to address the trauma as soon as possible rather than waiting for your symptoms to worsen. Social support during this time is crucial, too.
But if your trauma does develop into ASD or PTSD, help is available. The courses of treatment for both conditions are similar. Two main modalities are used: therapy and psychiatric medications. Oftentimes, a combination of therapy and meds is used for the most effective outcome.
Working with a trauma-informed therapist is essential when treating PTSD or ASD. A few of the most common types of therapy for trauma, ASD, and PTSD include:
Join the Charlie Health Library
Get mental health updates, research, insights, and resources directly to your inbox.
You can unsubscribe anytime.
Cognitive behavioral therapy (CBT)
CBT can help you become more aware of your thoughts, feelings, and behaviors –– how they all interact with one another. You will learn ways to deal with tough emotions and cope with stress, in addition to recognizing problematic thoughts and behaviors and replacing them with healthier ones.
Exposure therapy
Trauma might make you avoid particular situations, things, people, or even memories that make you recall the traumatic event or events you endured. With the assistance of a mental health professional, exposure therapy can help you safely revisit triggers. You can work towards desensitizing yourself to these triggers and memories with a trauma-informed therapist who you trust.
Eye movement desensitization and reprocessing (EMDR)
EMDR is a unique treatment that makes use of your eye movements to help you process difficult memories linked to your trauma. With this type of therapy, you may be able to process trauma faster.
When it comes to medications, the most common meds prescribed for ASD and PTSD are antidepressants and anti-anxiety drugs. The ideal medication or combination of meds for your particular circumstance may require some patience and trial and error. When determining your treatment plan, your doctor will also take into account any additional co-occurring mental health conditions.
On top of working with a mental health professional or team of professionals, it’s important to take care of yourself on your own time by incorporating self-care into your routine. Some ways you can do this are:
- Remaining physically active, aiming for at least 15 minutes of activity every day
- Eating a healthy and balanced diet
- Getting enough high quality sleep
- Abstaining from alcohol and drugs
- Having a creative outlet for your emotions, such as music or art
- Meditating or practicing mindfulness
- Relying on a strong social support system
How Charlie Health can help
If you’ve experienced trauma, you are far from alone. Trauma is unfortunately common, with an estimated 50% of women and 60% of men going through at least one traumatic event in their life.
Traumatic incidents affect everyone differently. Some people may seemingly bounce back pretty quickly after trauma, while others may experience long-term mental health struggles like post traumatic stress disorder (PTSD).
Regardless, plenty of research has shown that whether you realize it or not, trauma directly affects your brain. For example, if you experienced childhood trauma or complex trauma growing up, it’s very possible that your brain development was affected. Trauma in adulthood can also result in a variety of changes to the brain. If you’re a teen or young adult who has experienced trauma –– or if you think you might have acute stress disorder or post traumatic stress disorder –– Charlie Health may be able to help.
Our personalized intensive outpatient program offers mental health treatment for teens, young adults, and families dealing with a variety of struggles, including trauma, ASD, and PTSD. In our program, you will be matched with a therapist who meets your specific needs, and connected with a group of peers from similar backgrounds with similar struggles to help you remember you are not alone.
Coping with trauma can be difficult, but with treatment and dedication, you can push forward, heal, and grow from trauma. Help is here now. We're available 24/7 to get you started on your healing journey.
References
https://www.ncbi.nlm.nih.gov/books/NBK537102/
https://www.health.harvard.edu/staying-healthy/understanding-the-stress-response
https://jamanetwork.com/journals/jamapsychiatry/fullarticle/1389371
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3548359/
https://www.britannica.com/science/hippocampus
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8170416/
https://www.sciencedirect.com/topics/medicine-and-dentistry/prefrontal-cortex
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2738354/
https://www.ncbi.nlm.nih.gov/books/NBK519704/table/ch3.t30/
https://www.ncbi.nlm.nih.gov/books/NBK207191/box/part1_ch3.box16/
https://my.clevelandclinic.org/health/articles/22513-neurotransmitters#
https://www.childwelfare.gov/pubpdfs/braindevtrauma.pdf
https://www.sciencedirect.com/science/article/pii/S0896627316000209