
Table of Contents
Let’s Talk About Perinatal Mood and Anxiety Disorders
Written By: Charlie Health Editorial Team

Clinically Reviewed By: Dr. Don Gasparini
December 22, 2023
5 min.
If you or a loved one are struggling with mental health symptoms during pregnancy and postpartum, you’re far from alone, and help is available.
Learn more about our Clinical Review Process
Table of Contents
During the pregnancy and postpartum period, about a quarter of people will develop a mood or anxiety disorder, known collectively as perinatal mood and anxiety disorders (PMADs). Despite being relatively common and treatable, PMADs often go undiagnosed and untreated, especially among marginalized populations. Below, we delve into everything you need to know about PMADs, including the signs and symptoms of different perinatal mental health conditions, ways to cope, and how to find actually effective treatment.

Check out our maternal mental health program
Personalized, virtual care with other new parents.
What are the types of perinatal mood and anxiety disorders?
As mentioned, PMADs are a range of mental health conditions that can occur during pregnancy and the postpartum period (known collectively as the perinatal period, hence the name). Below are some of the most common types of PMADs.
Postpartum depression
Perhaps the most well-known perinatal mood disorder, postpartum depression affects about one in seven people in the year after birth. The condition is marked by persistent feelings of sadness, fatigue, changes in appetite, and difficulty bonding with the newborn and can also develop during pregnancy (which is why the condition is increasingly referred to as perinatal depression).
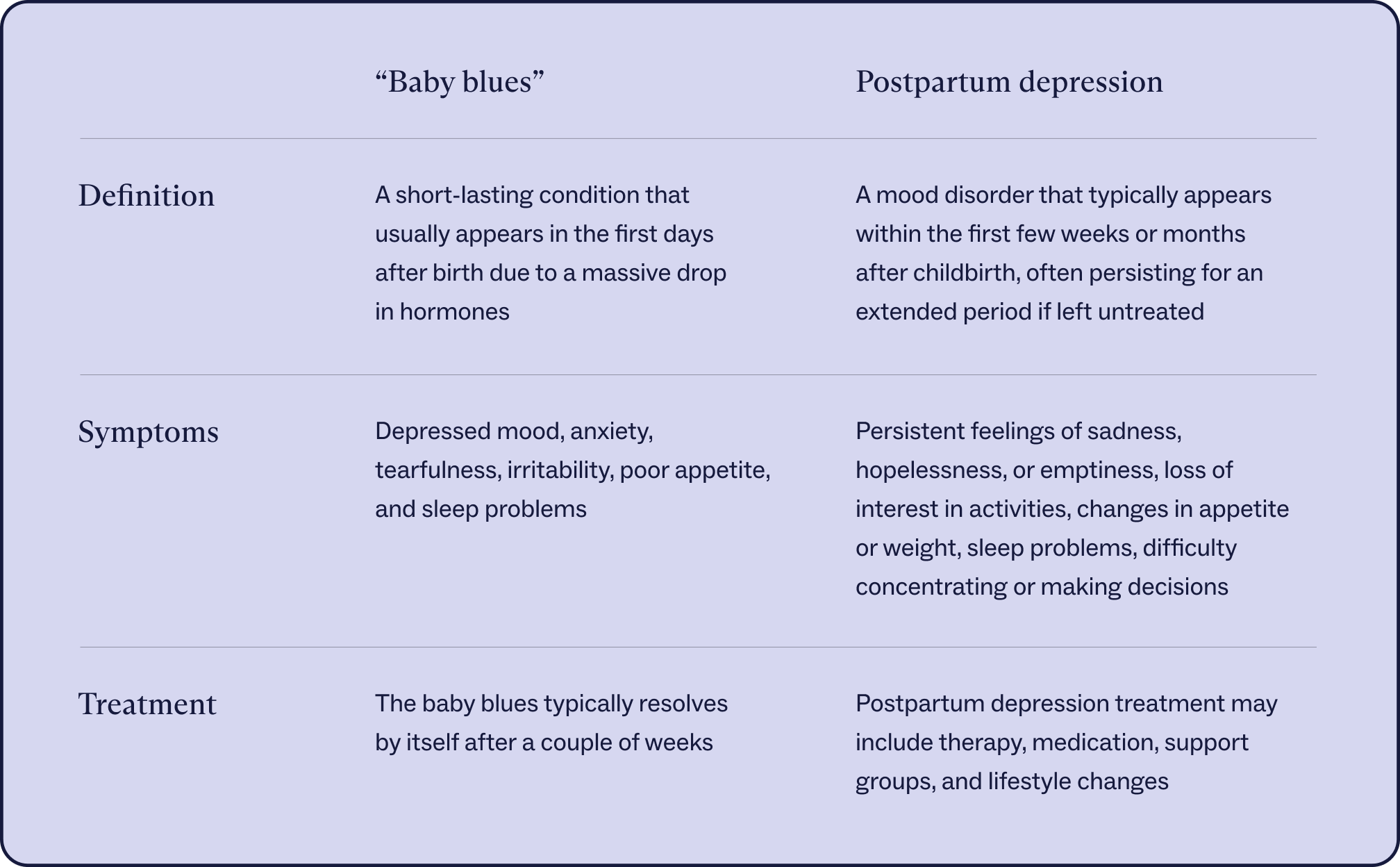
Postpartum depression is different from the “baby blues,” a common emotional response in the first days after birth. Though the baby blues symptoms are similar to postpartum depression (depressed mood, anxiety, tearfulness, irritability, poor appetite, and sleep problems), the former is not considered a PMAD because it usually resolves by itself after a couple of weeks. Postpartum depression and other PMADs, by contrast, usually require treatment. Rates of postpartum depression, though, are higher in those with postpartum baby blues, with up to one-quarter of baby blues patients going on to develop postpartum depression, data shows.

How Dejah J. Managed Postpartum Depression With Charlie Health
Charlie Health Editorial Team
Postpartum anxiety
Intensive and persistent fears and worries that develop in the weeks and months following childbirth and interfere with daily functioning are known as postpartum anxiety. In addition to excessive worry, symptoms of postpartum anxiety may include restlessness, irritability, intrusive thoughts, and physical symptoms like trembling or nausea. Like postpartum depression, the condition can also develop during pregnancy, which is why some call it perinatal anxiety. Many cases of postpartum anxiety go undiagnosed, making it hard to pinpoint the prevalence of the condition, but most studies estimate rates are about 11% to 21% after birth in the United States.
Postpartum obsessive-compulsive disorder (OCD)
A form of OCD that (as its name suggests) develops during the postpartum period, usually defined as the first 12 months after a baby is born. Studies show that up to about one-quarter of the postpartum population may experience postpartum OCD, but among those with existing OCD, pregnancy and postpartum may exacerbate symptoms for up to 70% of people. Like typical OCD, postpartum OCD is marked by intrusive thoughts or images (obsessions) and mental or physical rituals (compulsions) in response to the intrusive thoughts.
The obsessions associated with postpartum OCD often include illogical thoughts and compulsions related to infant harm—also a common feature of postpartum psychosis, a more severe and rare condition that more commonly results in actual harm (more on this below). If you’re having thoughts of harming yourself or someone else, including an infant, this is a mental health emergency, and you should contact The Suicide & Crisis Lifeline by calling or texting 988.
Postpartum post-traumatic stress disorder (PTSD)
This condition most commonly occurs after a traumatic childbirth experience and may involve symptoms such as intrusive memories, nightmares, and hypervigilance.
Postpartum psychosis
A severe and rare condition characterized by hallucinations, delusions, and extreme mood swings, including thoughts of harm to oneself and one’s baby. Postpartum psychosis requires immediate medical attention. Although it is serious, postpartum psychosis is relatively rare. Perinatal psychiatric hospital admissions affect less than 1% of first births, data shows.
What causes PMADs to develop during pregnancy and postpartum?
The causes of PMADs vary from person to person, but biological, psychosocial, and social factors are believed to play a role. Hormonal changes during pregnancy and postpartum are believed to be a leading cause of why people are more likely to develop depression and anxiety in the year after childbirth than at any other time in their lives. Genetics and biology also play a role. People with a personal or family history of mood or anxiety disorders face an increased risk of developing PMADs, research shows.
Lastly, those who deal with higher levels of stress, a history of trauma, or pregnancy or childbirth complications are all considered to be more at risk for PMADs. Not all people with these risk factors will develop PMADs, though, and people can develop the condition without these risk factors.
Effective treatment for PMADs
Since PMADs encompass a range of conditions, the most effective treatment for each condition (and person) will vary. Most treatment plans, though, will include therapy and medication (as needed).
Cognitive behavioral therapy (CBT) is widely used to help people change negative thoughts about pregnancy and parenting and teach healthier coping and behavioral skills. CBT and other therapeutic interventions can be used to treat PMADs in individual or group settings. Supported groups and group sessions create a sense of community and shared experience, reducing the isolation and stigma often faced by people with PMADs.

Medications may also be recommended to treat certain PMADs, including antidepressants or anti-anxiety medications prescribed under the guidance of a psychiatrist or healthcare provider. Some people with PMADs may benefit from specialized care from perinatal psychiatrists who have expertise in the unique mental health challenges associated with pregnancy and postpartum.
PMADs treatment at Charlie Health
If you or a loved one are struggling with PMADs, Charlie Health is here to help. Charlie Health’s virtual Intensive Outpatient Program (IOP) includes an accessible, curated maternal mental health program for perinatal and postpartum clients. Our expert clinicians incorporate evidence-based therapies into individual counseling, family therapy, and group sessions. With treatment, managing your mental health during pregnancy and postpartum is possible. Fill out the form below or give us a call to start healing today with our maternal mental health program.
References
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4369539/
https://pubmed.ncbi.nlm.nih.gov/11995777/
https://jamanetwork.com/journals/jamapsychiatry/fullarticle/209983
https://link.springer.com/article/10.1007/s11920-022-01333-4
https://www.sciencedirect.com/science/article/abs/pii/S1555415520304529
https://www.tandfonline.com/doi/abs/10.1080/j.1600-0412.2001.080003251.x
https://www.ncbi.nlm.nih.gov/books/NBK519070/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10050873/
https://www.psychiatrist.com/jcp/the-perinatal-depression-treatment-cascade/




