
Table of Contents
Here’s What Not to Say to Someone With Depression

Written By: Ethan Cohen BSN, RN

Clinically Reviewed By: Dr. Don Gasparini
January 4, 2024
6 min.
You’ll want to steer clear of “try not to think about it” and “you don't seem depressed.”
Learn more about our Clinical Review Process
Table of Contents
According to research by the National Institute of Mental Health (NIMH), about one in five adolescents (20.1%) and just under one in 10 adults (8.3%) experienced a major depressive episode in 2021. Based on these statistics, it is more than likely that you have at least one friend or loved one who has struggled with depression at some point in their life.
If that’s the case, you may be asking how best to support a loved one suffering from depression. Of course, your intentions to help them are good, but without a proper understanding of the mental health issue and its impact on a person’s life, it’s possible to accidentally say something insensitive. Keep reading to learn more about what not to say to a loved one with depression.

We’re here to help your loved one
Virtual, intensive care for depression without a waiting list.
5 things not to say to someone with depression
Words play an important role in supporting someone with depression. Thoughtful and validating communication can provide comfort, reassurance, and a sense of being heard. However, careless or dismissive language can contribute to feelings of isolation, anger, hopelessness, and frustration that someone with depression is already experiencing.
Simply put, the words we use impact how people with depression feel and perceive support, shaping their path to healing. Below, we debunk some common misconceptions about depression and give five examples of things you should not say to someone dealing with the condition.
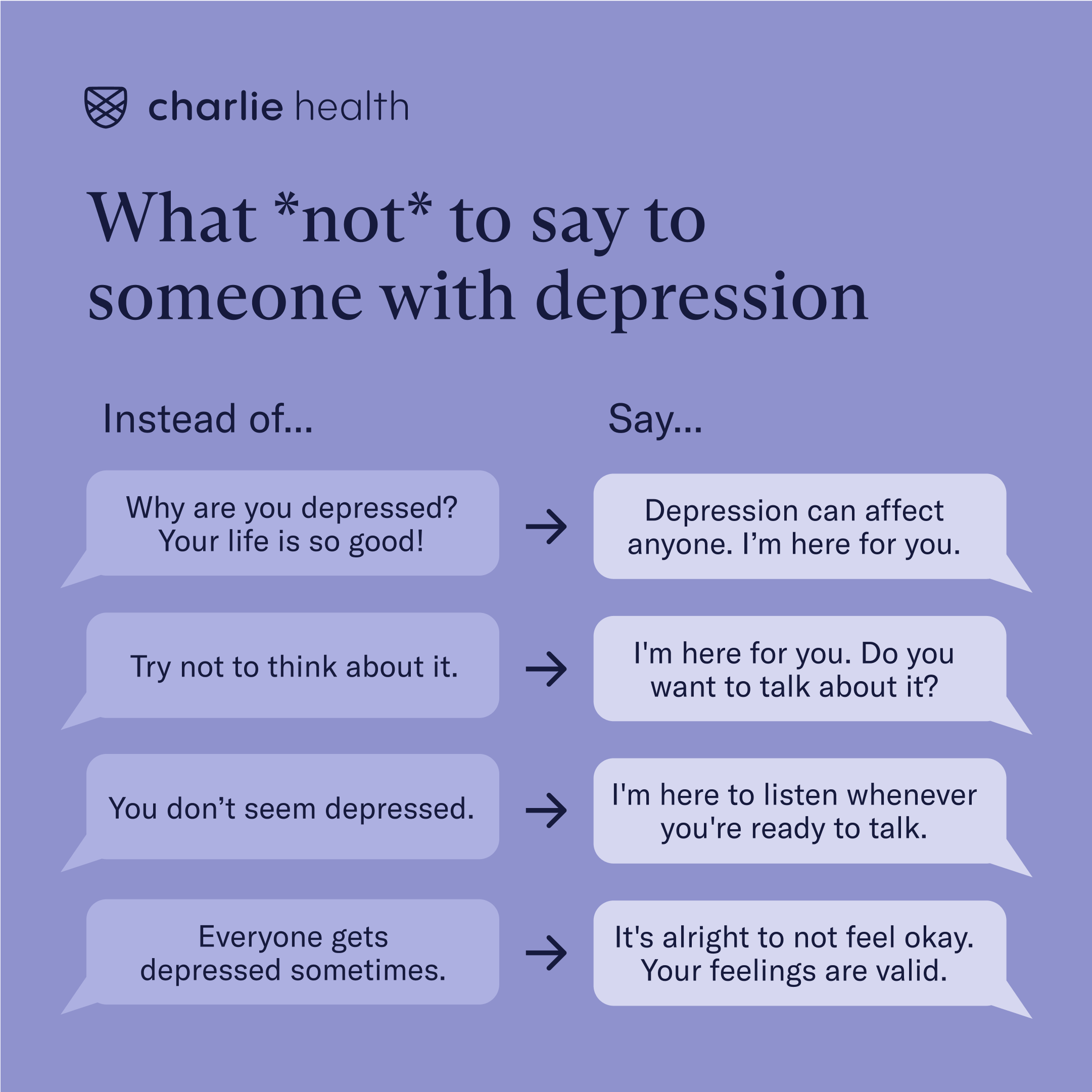
1. “Why are you depressed? Your life is so good!”
A common misconception about depression is that it only happens when someone is going through an emotionally difficult time. While it is the case that certain situations, such as a traumatic event or the loss of a loved one, can lead a person to develop depression, it is also true that depression can happen when a person’s life is full of so-called good things.
Take postpartum depression, for instance, a common form of depression affecting one in seven birthing people in the year after childbirth. Society has created an expectation that the postpartum period is one of joy and happiness, so it may be challenging for some people to understand why a new parent feels persistent sadness and struggles to bond with their newborn.
In reality, there are many causes of depression beyond life events, like genetics and brain-related mood dysregulation, and it’s important to keep this in mind when supporting a depressed person. Instead of suggesting someone’s seemingly positive life experiences negate their negative emotions, try validating the depressed feelings that they’re sharing with you.
2. “Try not to think about it.”
While this may be intended as helpful advice, it’s not actually possible for people with depression to just “not think about” their negative thoughts and feelings. Many people with depression struggle with a symptom known as toxic rumination, a cycle of repetitive negative thinking that can affect someone’s body and mind. It’s usually not possible for depressed people to will themselves out of the cycle of toxic rumination, and suggesting that they do so may feel insensitive.
Instead of suggesting that your loved one try to think of something else, a better suggestion would be to ask them if they would like to see a movie, play a game, or just have a conversation that is light and easy. Studies have shown that distraction is one of the most powerful tools a person can use when attempting to quiet negative thoughts and feelings in the context of toxic rumination. Keep in mind that if your loved one is not interested in participating, pushing your suggestion on them with too much force can be counterproductive.
3. “You don’t seem depressed.”
Depression is often depicted as the total inability to get out of bed or accomplish any tasks, and while that’s sometimes the case, the condition may present with more subtle signs. For example, it may be the case that your loved one is experiencing atypical depression (colloquially known as “smiling depression”), a subtype of major depressive disorder with depressive symptoms that improve in response to positive events. Basically, some people with depression maintain a cheerful exterior but are actually dealing with internal turmoil and need support.

It’s crucial not to discount someone’s experience of depression based on their outward appearance. Instead of relying on visual cues, try to engage in open conversations, expressing genuine concern and care for their well-being. Recognizing the nuanced nature of depression can help you take a more empathetic approach, fostering genuine support and trust.
4. “Everyone gets depressed sometimes. You’ll feel better eventually.”
Feeling occasionally sad or down is different than having clinical depression—a common but serious mood disorder that affects how a person feels, thinks, and handles their day-to-day life and often requires professional intervention. While you may be trying to reassure a loved one that everything will be okay, saying something like this can minimize their experience of depression. For instance, many people with severe depression struggle with suicidal thoughts or thoughts of self-harm, a markedly different experience than passing sadness.
Instead of suggesting that a loved one’s depression will resolve on its own, consider helping them connect with necessary mental health resources. Also, if a loved one indicates that they are thinking about harming themselves or someone else, this is a mental health emergency, and you should contact The Suicide & Crisis Lifeline 24/7 by calling or texting 988. If they’re not in crisis and don’t need support from a national suicide prevention lifeline, you could encourage them to reach out to a mental health professional—and even support them in doing so if they want your help.
5. “When I was depressed, I started doing yoga, and things got better right away!”
While sharing your own experience with depression may seem like a helpful thing to do, more often than not, statements like these may not help because what works best for one person may not work for another. Different forms of depression require different therapeutic interventions, and mental health treatment should be tailored to the individual.
Instead of giving unsolicited advice, express empathy towards your loved ones’ situation and ask what things make them feel better (if only a bit). While research shows that lifestyle changes like regular exercise and good sleep hygiene can help with depression symptom management, every person is different, and what makes one person feel good may not work for another.
If a loved one is looking for treatment advice, it’s best to encourage them to contact a mental health professional (as discussed). Although depressive symptoms may get better with lifestyle changes and support from loved ones, depression is a mental health issue that often doesn’t improve without professional support.

Depression treatment at Charlie Health
If depression symptoms are impacting your mental health, Charlie Health is here to help. Charlie Health’s virtual Intensive Outpatient Program (IOP) provides more than once-weekly mental health treatment for young people dealing with complex mental health conditions, including clinical depression. Our expert clinicians incorporate evidence-based therapies into individual counseling, family therapy, and group sessions. With treatment, managing your depression symptoms is possible. Fill out the form below or give us a call to start healing today.
References
https://www.psycom.net/depression/what-not-to-say-to-someone-with-depression
https://www.nimh.nih.gov/health/publications/depression
https://www.medicalnewstoday.com/articles/what-to-say-to-someone-who-is-depressed#what-to-say
https://www.nimh.nih.gov/health/statistics/major-depression
https://www.samhsa.gov/mental-health/how-to-talk/friends-and-family-members
https://www.psychiatry.org/patients-families/helping-a-loved-one-cope-with-mental-illness




