
Table of Contents
Unipolar Depression: Definition, Symptoms, and Treatment

Written By: Alex Bachert, MPH

Clinically Reviewed By: Dr. Don Gasparini
April 21, 2022
6 min.
Unipolar depression is a significant mental health disorder facing teens today. We outline what causes it, how to identify it, and the treatment for the disorder.
Learn more about our Clinical Review Process
Table of Contents
WARNING: this post contains in-depth language and information about suicide. If you are in acute crisis looking for help, please call the National Suicide Prevention Lifeline at 988 or dial 911.
Unipolar depression—also known as major depressive disorder or clinical depression—can be overwhelming for anyone in its shadow. It’s different from feeling down over a breakup or frustrated by something that happened at school. Instead, it’s a serious mood disorder with physical and psychological symptoms that can interfere with how you feel, function, and live your everyday life.
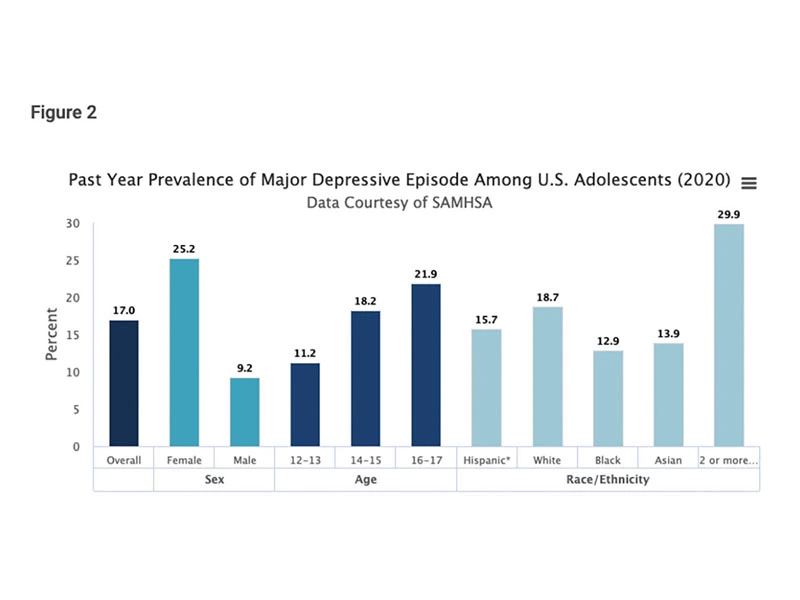
It’s quite possible that you know someone with unipolar depression. According to the National Institute of Mental Health, unipolar depression is one of the most common mental health disorders in the United States, affecting nearly 17 percent of the U.S. population aged 12 to 17 years in 2020. This means that approximately 4.1 million adolescents experienced at least one unipolar depressive episode that year. To make it worse, less than half (41.6 percent) of teens who experienced a unipolar depressive episode received treatment.
Aside from the immediate side effects of depression, unipolar depression is a mental disorder that can have serious consequences on academic performance, social functioning, and suicidal risk factors when left untreated in adolescents. Suicide rates among teens have steadily increased over the last decade, and suicide was the second leading cause of death among adolescents and young adults in 2019.
That’s why Charlie Health believes it’s so important to empower teens, young adults, and families to explore their mental health through accessible resources and information. Below, we’ve broken down the research on symptoms, causes, and treatments to support your journey in better understanding unipolar depression.
What is unipolar depression?
Unipolar depression is a type of mood disorder characterized by depressive symptoms such as persistent feelings of sadness, hopelessness, worthlessness, and low mood. Unlike bipolar depression, which includes cycles of manic symptoms and depressive episodes, unipolar depression consists entirely of depressive episodes. This means that individuals with unipolar depression do not experience manic or hypomanic episodes. Unipolar depression can be severe and significantly impact an individual’s ability to function in daily life. It can also increase the risk of suicide, making it important for individuals to seek professional help if they are experiencing unipolar depression symptoms.
Join the Charlie Health Library
Get mental health updates, research, insights, and resources directly to your inbox.
You can unsubscribe anytime.
What are the symptoms of unipolar depression?
Unipolar depression is a mental health condition that is unique to each person, so not everyone with the condition will experience the same symptoms. The symptoms, however, will always be severe enough to cause a noticeable difference in how someone functions day-to-day.
Unipolar depression is diagnosed when a person experiences five or more of the following depressive symptoms on most days for at least two weeks.
- Persistent feelings of sadness, hopelessness, or emptiness
- Loss of interest or pleasure in most activities
- Significant changes in appetite or weight
- Sleep disturbances, either sleeping too much or too little
- Restlessness or slowed down
- Loss of energy or fatigue
- Feelings of worthlessness or guilt
- Difficulty concentrating or making decisions
- Recurrent thoughts of death or suicidal thoughts
Unipolar depression causes and risk factors
Now that you have a better understanding of the signs and symptoms, you might be asking yourself what causes unipolar depression. Depression is a complex condition that can occur for a variety of reasons—ranging from your biology to your biography. According to the National Institute of Mental Health, clinical depression is often caused by a combination of environmental, psychological, and genetic factors.
Family history: Research suggests that individuals whose parents were diagnosed with a psychiatric disorder are at significantly greater risk of developing unipolar depression themselves. The data also found that factors such as substance use, poor academic performance, poor parent-child relationship, and childhood abuse by age 11 increased the risk of a unipolar depression diagnosis.
Habits and lifestyle: Smoking, alcohol use, high BMI, poor sleep, and sedentary behavior have all been linked to increased rates of unipolar depression in adolescents. Results from a 2020 national study suggest that among individuals who engaged in these habits, the prevalence of unipolar depression significantly increased among adolescents from 13 years to 16 years and was more common among females.
Life events: Major milestones can be a time of joy and celebration (think: getting married, having a baby, starting a new job), but they can also mark less happy occasions. Events such as death of a loved one, financial debt, and even romantic rejection can all lead to depressive episodes. And while feeling down due to these events is completely normal, these events can further exacerbate the pain for those already living with depression.
Physical conditions and medications: Physical illnesses—such as stroke, heart disease, and other chronic conditions that cause pain or discomfort—can increase a person’s risk of developing severe depression. The same goes for certain drugs, including isotretinoin (used to treat acne), steroids, and a smoking cessation drug called varenicline; however, it’s always best to discuss the benefits and risks with your healthcare provider.
Unipolar depression diagnosis
A unipolar diagnosis is often based on several factors. Your healthcare provider may conduct a physical exam and blood work in order to rule out any underlying health problems that could be causing the symptoms. You’ll also be asked to complete a self-reported psychiatric evaluation, such as a Patient Health Questionnaire-9 (PHQ-9), so that your provider can better understand your symptoms, thoughts, feelings and behaviors.
Do you need more support with
your mental health?
Charlie Health can help.
How do you treat unipolar depression?
Fortunately, unipolar depression treatment is manageable with access to therapy, psychiatric medications, and lifestyle changes. And in fact, treatment with both medications and psychotherapy has been found to be more effective than either of these treatments on their own.
Medication for depression
The prescription medication used to treat depression is called an antidepressant. They're a treatment option designed to balance the levels of chemicals in our brain called neurotransmitters, which can help to improve mood and functioning. We’ve listed several categories of antidepressant medication below, but it’s best to speak with a healthcare provider to learn more about the best treatment option for you.
- Serotonin reuptake inhibitors (SSRIs)
- Serotonin and norepinephrine reuptake inhibitors (SNRIs)
- Tricyclic antidepressants (TCAs)
- Monoamine oxidase inhibitors (MAOIs)
Therapy for unipolar depression
There are several therapy options for individuals living with unipolar depression and choosing the right one often boils down to the severity of the symptoms and/or condition. Charlie Health’s intensive outpatient therapy programs are designed to offer individualized treatment plans based on specific needs and preferences. Whether it is cognitive behavioral therapy (CBT), dialectical behavior therapy (DBT) skills, or mindfulness practices, our patients will have the evidence-based treatment modalities they need to work toward a successful recovery.
Below are some additional ways to help anyone who is struggling with depression to improve their quality of life.
Peer support groups: Support groups can be a great way for individuals with unipolar depression to share their experiences and learn helpful tips for coping with depression.
Helplines: If you or someone you know is experiencing a mental health crisis related to unipolar depression, the National Suicide Prevention Lifeline is always available. Call them at 988 or text the Crisis Text Line at HOME to 741741.
Seek support with Charlie Health
Most individuals who experience a single episode of unipolar depression will likely experience additional episodes or co-occurring mental health conditions. Medication, lifestyle changes, and a supportive group of family and friends are so helpful for coping with depressive episodes, but it’s not always enough.
Charlie Health’s intensive outpatient program (IOP) connects each client with a licensed therapist based on their individual needs, preferences, background, and experiences to promote healing in a safe, supportive space. Therapy may sound daunting, but the Charlie Health community is here for you each step of the way.
To learn more, read our blog about the major types of depression in teens and young adults here.
References
NIMH, Past Year Prevalence of Major Depressive Episode Among U.S. Adolescents (2020)
https://www.nimh.nih.gov/health/statistics/major-depression
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6213890/
https://www.nimh.nih.gov/health/topics/depression
https://www.psychiatry.org/patients-families/depression/what-is-depression
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4244653/
https://pubmed.ncbi.nlm.nih.gov/32448926/e
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181771/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2729620/





