
Table of Contents
New Research: Virtual IOP Helps Improve Teen Depression

Written By: Alex Bachert, MPH

Clinically Reviewed By: Dr. Kate Gliske
April 13, 2023
5 min.
Virtual intensive outpatient programming is an effective alternative to in-person mental health treatment, especially for LGBTQIA+ youth and other marginalized individuals.
Learn more about our Clinical Review Process
Table of Contents
Accessing mental health services isn’t always simple for teens, young adults, and their families. Between mental health provider shortages and excessive wait times, barriers to care sometimes prevent people from receiving the treatment they need. Currently, only 39% of hospital-based facilities nationwide serve teens under 18 years, and the average wait time for youth-serving facilities is 6-8 weeks.
Another predicament for teens and young adults who are seeking mental health care is a dearth of developmentally-appropriate treatment options. Some research shows that only 36% of mental health programs are designed specifically for children and adolescents, and just 22% are designed for transition-age young adults.

We know that intensive outpatient programming (IOP) is an effective option for treating youth with complex mental health needs. Still, in-person IOP is often limited to clients who live locally and have the flexibility to visit a clinical setting several days per week. So is it possible to take the concept of in-person IOP and make it virtual? The answer—of course—is yes, but Charlie Health believes in showing the evidence to support its mission of creating equitable access to mental health services.
In order to understand the effectiveness of virtual IOP as an alternative to in-person IOP, a team of researchers looked at how teens and young adults rated their depression at the start and end of virtual IOP at Charlie Health. Continue reading to learn how this newly-published peer-reviewed research supports the idea of using virtual treatment to improve access to care, as well as everything you need to know about intensive outpatient programming. Read the full publication here.
The research: is virtual IOP effective?
A team of researchers—including Dr. Caroline Fenkel, DSW, LCSW, Co-Founder and Chief Clinical Officer at Charlie Health and Bethany Peralta, CMA, RMA, Clinical Outcomes Analyst at Charlie Health—conducted a nationwide study to understand the effectiveness of a virtual IOP program to treat depression in adolescents and young adults.
The study included more than 1,000 people ages 11-25 years from 14 states who participated in Charlie Health’s IOP between June 2021 and October 2022. To be eligible for the study, all individuals were required to have a depressive disorder diagnosis and have had spent at least 18 hours (which equals seven sessions) and two weeks in care.
Let’s take a look at the study participants.
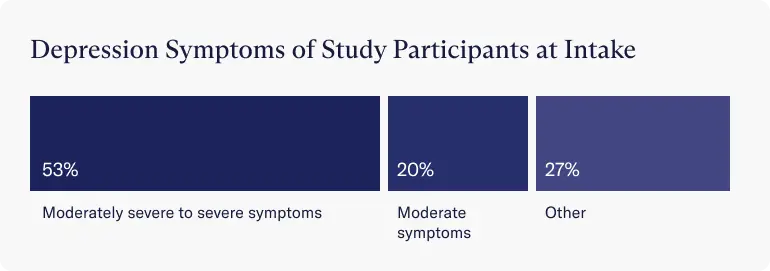
- The average age was 16 years. Over half of people entered treatment with moderately severe to severe depression symptoms (53%) and another 20% reported moderate symptoms.
- Almost half of the people identified as female (44%), 23% identified outside of the male/female binary, and 20% identified as transgender.
- A majority of the people (60%) identified as a member of an LGBTQIA+ community, with 30% identifying as heterosexual.


The findings: virtual IOP effectively treats depression in youth
The study concluded that virtual IOP is an effective alternative to in-person mental health treatment for teens and young adults with depression, especially for those from marginalized groups. These findings support a growing body of evidence suggesting that mental health needs can be effectively met using remote treatment models. It also supports the idea of using virtual treatment for individuals with more complex mental health needs.
Decrease in depression scores
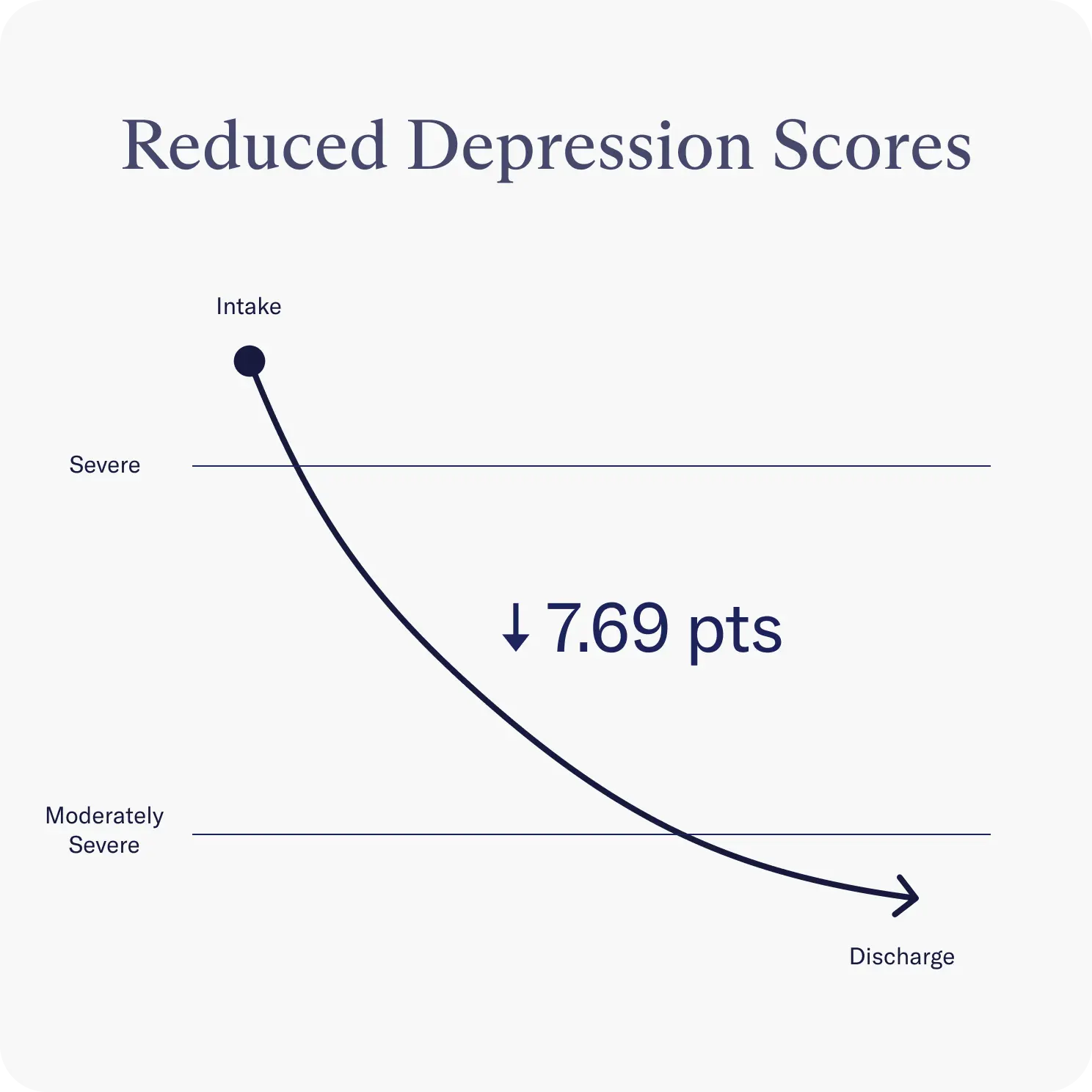
Depression was measured using a PHQ-A, a multiple-choice self-report questionnaire that monitors depression severity. The researchers found that youth in the virtual IOP saw a significant decrease in depression between intake and discharge, and noted that many individuals were even able to move below the clinical cutoff for major depressive disorder between starting and finishing the treatment program.
Equitable access and care
The study also found that virtual IOP is an equally effective treatment for adolescents and young adults across all gender and sexual orientation populations. This is especially important since marginalized populations—such as LGBTQIA+ individuals (lesbian, gay, bisexual, transgender, queer, questioning, intersex, and asexual/aromantic/agender, plus all other identities along the gender and sexuality spectrum)—are at higher risk of mental health disorders and tend to face even greater barriers to appropriate mental health services than non-marginalized groups.
Other benefits of virtual IOP
The researchers went on to list additional benefits of virtual IOP, including:
- Virtual programs make it easier for teens and young adults to connect with like-minded peers, which isn’t always feasible with place-based programs. This is particularly helpful for LGBTQIA+ individuals.
- Since virtual care includes youth from across the country, it’s possible to create treatment groups that are the ideal therapeutic size and based on the same diagnoses, symptoms, and stage of development—a challenge when limited by location.
- Virtual care offers more flexibility for parents who want to be involved in their child’s treatment, without having to worry about time off of work or commuting to a clinic.
What should I know about IOP?
Intensive outpatient programming (IOP) is a form of treatment used to help people living with mental and behavioral health conditions. Usually, this means depression, anxiety disorders, trauma, mood disorders, self-harm, and other behavioral issues.
IOP is designed for individuals who need more support than they’d get through traditional outpatient services, but don’t require 24/7 care like they’d receive with residential or inpatient treatment. Generally speaking, there are two main reasons a person would enroll in an IOP:
- A recent discharge from a residential treatment program or emergency department
- They already attend weekly therapy but are still struggling with their mental health and would like additional support
IOP is considered to be particularly beneficial for youth and young adults because it offers them a chance to receive the care they need while still maintaining a sense of normality. Going to school or work, maintaining friendships, and exploring hobbies and interests are all doable—and encouraged—while participating in an IOP.
IOP typically lasts 9-12 weeks and includes:
- 1 hour of individual therapy per week
- 1-2 hours of family therapy per week
- 3 hours of supported groups, 3 days per week
In-person IOP vs. virtual IOP
The primary difference (and benefit) of virtual IOP is that it removes the geographic barrier to care. While in-person programs require young adults and their families to live locally or endure lengthy commutes, virtual programs bring the care right to each family.
Get help today
If you or someone you know might benefit from a higher level of mental healthcare, Charlie Health is here to help. Founded in 2020, Charlie Health is the largest virtual mental health clinic for teens and young adults who are struggling with depression and other serious mental health disorders. Our program consists of individual therapy, family therapy, and support groups in order to best meet the needs of each person—all from your home.
Whether you’re exploring treatment options for the first time or looking for additional support, Charlie Health can offer you individualized and evidence-based mental health care in a safe, supportive space.
Reach out to learn more today.
References
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4833684/
https://www.samhsa.gov/data/quick-statistics-results?qs_type=nmhss&state=United%20States&year=2017
https://psycnet.apa.org/record/2008-11685-002
https://pubmed.ncbi.nlm.nih.gov/26465266/
https://www.charliehealth.com/post/what-is-lgbtqia-counseling





